Clinical Research
(CR-017) Closing the gap on racial disparities in the diagnosis of chronic wound infections: the concerning trend involving skin pigmentation and a role for fluorescence imaging
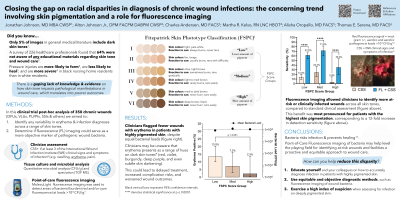
Skin pigmentation has a negative impact on the ability to diagnose skin pathology. In skin pathology and wound care, diagnostic indicators (e.g. cyanosis, inflammation, blanching) vary considerably depending on the level of melanin. Erythema, a key indicator of wound infection, presents differently on dark skin and is often missed when assessing high melanin content chronic wounds. Using a 14-site, 350 wound study (DFUs, VLUs, PIs, surgical wounds), we investigated how the reporting of clinical signs/symptoms of infection (including erythema) differs based on skin tone, and whether fluorescence imaging can offer a more equitable solution for detecting infection-causing bacteria in wounds.
Methods:
In this post-hoc analysis of the FLAAG clinical trial participants were assigned to one of three groups, depending on their skin tone, as measured by the Fitzpatrick Scale: low (I & II), medium (III & IV), high (V & VI). Clinical signs and symptoms (CSS) of infection (IWII 2016 guidelines, ≥3 signs/symptoms or 1+ overwhelming sign/symptom) and total bacterial load (TBL) were compared across skin tones. Sensitivity for detection of TBL >104 CFU/g using clinical assessment alone and in combination with fluorescence imaging of wound bacteria were also compared.
Results:
Bacterial loads from biopsies did not differ across skin tone groups (Krushkal-Wallis test; p=0.38); median TBL was 106 CFU/g (range: 0 to 109). However, frequency of detected erythema decreased proportionally with increasing Fitzpatrick score, from 13.4% (low), to 7.2% (medium), to 2.3% (high), across a variety of wound types. Further, high Fitzpatrick-score group CSS sensitivity (2.9%) was 4.8-fold to 8.4-fold lower than low and medium groups (p=0.04-0.0025). Fluorescence imaging addition to clinical assessment improved detection of TBL >104 CFU/g in each of the Fitzpatrick groups (p< 0.0001); this improvement peaked in the “high” group at 12-fold over clinical assessment alone.
Discussion:
The ability to predict bacterial loads using CSS (including erythema) was significantly lower for patients with dark skin and increased by up to 12-fold after incorporating fluorescence imaging. This speaks to the racial disparities faced by wound care patients with dark skin, where missed diagnosis of pathogenic bacteria and infection could delay treatment, increasing the risk of complications and poor outcomes. Fluorescence imaging is poised to fill this gap, at least in part, and serve as a more objective and equitable indicator of wound bacteria.
Trademarked Items:
References:

.png)
