Case Series/Study
(CS-097) Zero Compromise to Clinical Outcomes, Improved Patient Experience in patients with complex wound utilizing an Innovative Negative Pressure Wound Therapy System.
Negative pressure wound therapy (NPWT) has become the go-to standard of care for complex wounds. Fournier’s gangrene (FG) affects 1.6 out of 100,000 people1 and treatment of FG is aggressive2. Research has shown that patients feel NPWT has a positive impact on their wound, however, patients also reported noise and mobility3. Long-term Acute Care Hospitals (LTACH) treat complex wounds, however the NPWT goal of therapy in LTACH’s is more often to decrease wound volume, increase granulation tissue and facilitate discharge to rehab or home health4. Complex wounds require high levels of staff skill when applying NPWT5.
The previous NPWT system at AMG was determined to be noisy, hinder mobility, had reliability issues and required additional documentation outside of the facility charting system. The AMG system evaluated an innovative NPWT system but would accept ZERO COMPROMISE to clinical outcomes.
Methods:
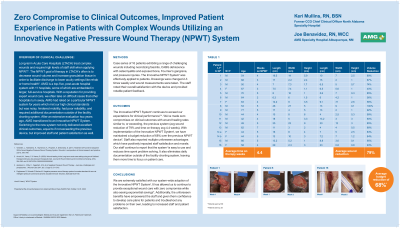
Case series of 16 patients exhibiting a range of challenging wounds included necrotizing fasciitis, CABG dehiscence with osteomyelitis and exposed bone, Fournier’s gangrene and pressure injuries. The innovative NPWT system was effectively applied to patients. Dressings were changed 2-3 times weekly and wound measurements were taken. The staff noted their overall satisfaction with the device and provided notable patient feedback.
Results:
Both the new and previous NPWT systems met the standard of care by maintaining set pressure at the wound site (EWMA)6 . This innovative system exceeded our expectations for clinical performance7, reliability and significantly reduced the burden of NPWT device documentation for billing and management. The results provided ZERO COMPROMIZE and exceeded expectations with wound reduction of averaging 79%. Time on therapy averaged 4.4 weeks.
Discussion:
Overall patient and staff satisfaction with the innovative device was high. Our staff has continued to state that the new system has less time problem solving. The ease of use includes the eradication of daily documentation outside of the facility charting system. The innovative NPWT system has maintained a budget reduction of 68% over the previous NPWT device. More importantly the high standards for patient outcomes remain consistent with the innovative NPWT device since the implementation.
Trademarked Items:
References: 1. Broner, M. (2020). Overview of Fournier’s gangrene. Urologic Nursing, 40(6), 291-293, 298. doi:10.7257/1053-816X.2020.40.6.291
2. Doughty, D. B. & McNichol, L. L. (Eds.). (2016). Wound ostomy and continence nurses society core curriculum: Wound management. Wolters Kluwer.
3. Ubbink, D.T., Westerbos, S.J., Evans, D. et al. Topical negative pressure for treating chronic wounds. Cochrane Database Syst Rev. 2008; 16: 3, CD001898
4. Arnold, M., Yanez, C. & Yanez, B. (2020). Wound healing in the Long-term acute care setting using an air fluidized therapy/continuous low pressure therapeutic bed. Journal of Wound Ostomy and Incontinence Nursing, 47(3), 284-290. doi:10.1097/WON. 0000000000000646
5. Verbelen, J., Hoeksema, H., Heyneman, A., Pirayesh, A. & Monstrey, S. (2011). Treatment of Fournier's Gangrene With a Novel Negative Pressure Wound Therapy System. Wounds: A compendium of clinical research and practice, 23(11), 342–349.
6. Apelqvist, J., Willy, C., Fagerdah, A.M. et al. Negative Pressure Wound Therapy – overview, challenges and perspectives. J Wound Care 2017; 26: 3, Suppl 3, S1–S113.
7. Paglinawan R, Schwab P, Bechert K. Negative pressure wound therapy system Innovates standard of care via intelligent pressure control and dynamic exudate removal. Wounds. 2020;32(10):S1-S8.

.png)