Case Series/Study
(CS-131) Novel Treatment of an Enteroatmospheric Fistula with Transforming Powder Dressing (TPD)
Despite advances in surgical care, enteroatmospheric fistulas (EAFs) present a highly challenging and devastating problem in wound care therapy.1 Proper management of EAFs is critical to improving recovery and fistula healing, and requires rapid intervention to prevent sepsis.2 EAF standard of care (SOC) is variable and may include dressings, pouches, floating stoma, and negative pressure wound therapy (NPWT).3 As proper wound care management is vital to ensure wound healing and prevent sepsis, consideration for alternative treatments which promote wound healing, isolate the fistula for proper treatment, improve quality of life (QoL), and reduce overall healthcare costs must be considered.
Methods:
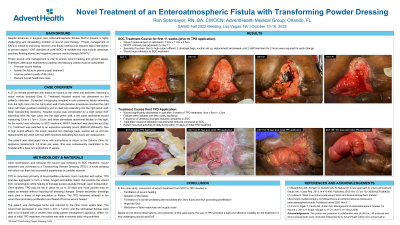
A 37-year-old female presented with extensive trauma to the chest and abdomen following a motor vehicle crash. Hospital course was complicated by a high output EAF extending from the right colon into the right pelvic wall, a left sided abdominal wound measuring 13cm x 11cm x 3.5cm, and three stomatized abdominal fistulae on the right.
NPWT treatment was initiated and subsequently discontinued. Treatment was switched to an expensive specialty pouch ($900-$1,200/each). Due to high output effluent, the pouch required 2 drainage bags, suction and replacement twice a week, requiring two staff members dedicating two-hours per replacement.
Results:
The patient was discharged home with instructions to return for appliance replacement 1-2 times per week. She was subsequently readmitted to the hospital with a fever and indications of sepsis. Upon readmission, wound treatment was changed to a novel Transforming Powder Dressing (TPD).
The patient was discharged home and returned to the clinic three weeks later. The wound had decreased in size (9cm x 8cm x 1.2cm), and the stomatized fistulae were able to be isolated with a smaller, less costly patient management appliance. Within 10-days of initial TPD treatment, the patient was able to resume daily living activities.
Discussion:
TPD is a novel dressing with which our team has successful experience in complex wounds. Upon hydration, TPD aggregated on the wound and formed a moist, oxygen-permeable matrix that protected the wound from contamination and helped manage excess exudate. Secondary dressings were used in areas of high exudation.
Treatment with TPD resulted in facilitation of wound healing, isolation of the fistula, improved QoL and a reduction in resource and supply costs. Based on the clinical observations and outcomes of this case study, use of TPD provided a safe and effective modality for the treatment of this challenging wound and EAF.
Trademarked Items:
References: 1. Meshikhes AW, Al-Hariri A, Al-Zahir AA, Al-Nahawi M. A rare approach to entero-atmospheric fistula. Am J Case Rep. 2013;14:476-480. Published 2013 Nov 13. doi:10.12659/AJCR.889638
2. Ludlow E. What is an Entero-cutaneous Fistula and Entero-atmospheric Fistula? https://www.insidescompany.com/blog/what-is-an-enterocutaneous-fistula-and-enteroatmospheric-fistula; Published online 2020 Nov 9
3. Terzi C, Egeli T, Canda AE, Arslan NC. Management of enteroatmospheric fistulae. Int Wound J. 2014;11 Suppl 1(Suppl 1):17-21. doi:10.1111/iwj.12288

.png)