Back
Case Series/Study
(CS-021) The Pattern of Use, and Presentation of A Case Series in Plastic Surgery, of a pHA* (pure Hypochlorous Acid) Preserved Wound Cleanser in an Acute Care Setting.
Co-Author(s):
<b>Introduction</b>: Several recent guidelines recommend the use of pure hypochlorous acid (pHA) based products for wound bed preparation. The high margin of safety associated with the product, combined with its evidence-based ability to remove colonization/biofilm and necrotic tissue, make it a compelling choice in our plastic surgery practice. Primary closure of wounds following good wound bed preparation practice reduces the burden on patients and our institution. Our use for this specific type of cleanser has increased from sporadic to routine.<br/><br/><b>Methods</b>: <div>
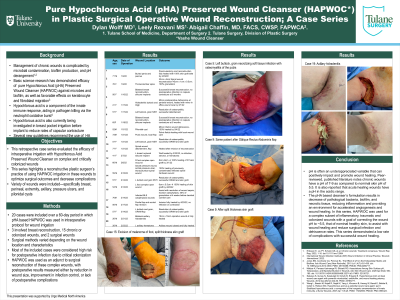
<p class="MsoNormal" style="margin: 0in 0in 8pt; line-height: 15.693333625793457px; font-size: 11pt; font-family: Calibri, sans-serif; caret-color: #000000; color: #000000; font-style: normal; font-variant-caps: normal; font-weight: normal; letter-spacing: normal; orphans: auto; text-align: start; text-indent: 0px; text-transform: none; white-space: normal; widows: auto; word-spacing: 0px; -webkit-text-size-adjust: auto; -webkit-text-stroke-width: 0px; text-decoration: none;"><span style="font-size: 14pt; line-height: 19.97333335876465px;">We present a quantitative view of our extent of adoption in a 60-day period, via retrospective chart review. We present 21 surgical patients, their wound etiologies, and wound closure times. We reviewed our EMR charts manually/electronically to obtain the extent of cleanser usage to augment our plastic surgery practice. In addition, we present several illustrative cases where visual images show the ability of the cleanser to eliminate visible slough/necrotic tissue.</span></p>
</div><br/><br/><b>Results</b>: <div>
<p class="MsoNormal" style="margin: 0in 0in 8pt; line-height: 15.693333625793457px; font-size: 11pt; font-family: Calibri, sans-serif; caret-color: #000000; color: #000000; font-style: normal; font-variant-caps: normal; font-weight: normal; letter-spacing: normal; orphans: auto; text-align: start; text-indent: 0px; text-transform: none; white-space: normal; widows: auto; word-spacing: 0px; -webkit-text-size-adjust: auto; -webkit-text-stroke-width: 0px; text-decoration: none;"><span style="font-size: 14pt; line-height: 19.97333335876465px; color: black;">There were zero postoperative infections. One patient with hypertension had a postoperative hematoma. Skin graft take was 100% for the foot wound skin grafts. Skin graft take was 90% for the pelvic NSTI patient, who had flap tip ischemic loss of about 5% of the flap after ER transfer for pulmonary complications. Other patients all healed uneventfully within the standard accepted postoperative time periods. The calciphylaxis patient achieved 40% granulation of his infected wounds within 3 weeks postoperative, and he had significant pain relief. However, his renal failure progressed and he elected to transition to hospice.</span></p>
</div><br/><br/><b>Discussion</b>: <div>
<p class="MsoNormal" style="margin: 0in 0in 8pt; line-height: 15.693333625793457px; font-size: 11pt; font-family: Calibri, sans-serif; caret-color: #000000; color: #000000; font-style: normal; font-variant-caps: normal; font-weight: normal; letter-spacing: normal; orphans: auto; text-align: start; text-indent: 0px; text-transform: none; white-space: normal; widows: auto; word-spacing: 0px; -webkit-text-size-adjust: auto; -webkit-text-stroke-width: 0px; text-decoration: none;"><span style="font-size: 14pt; line-height: 19.97333335876465px;">We have used evidence-based guidelines to guide our wound bed cleansing and preparation practice. Clinical and preclinical published data indicate that the safety and efficacy of the pHA based cleanser is high. Our high adoption rate is illustrated in the data. Wound bed preparation is based on wound visual inspection, sharp excisional debridement, occasional wound cultures, and irrigation and cleansing. We have used these techniques to prove, via the illustrative cases, that the use of pHA is a sound and safe way to achieve wound healing goals. </span></p>
</div><br/><br/><b>Trademarked Items</b>: <br/><br/><b>References</b>: 1. Armstrong DG, Bohn G, Glat P, Kavros SJ, Kirsner R, Snyder R, Tettelbach W.Armstrong DG, et al. Expert Recommendations for the Use of Hypochlorous Solution: Science and Clinical Application. Ostomy Wound Management 2015 May;61(5): S2-S19. https://pubmed.ncbi.nlm.nih.gov/28692424/
2. Block, Michael S, and Brian G Rowan. “Hypochlorous Acid: A Review.” Journal of Oral and Maxillofacial Surgery: official journal of the American Association of Oral and Maxillofacial Surgeons vol. 78,9 (2020): 1461-1466. https://europepmc.org/article/med/32653307
3. Dissemond J. Wound Cleansing: benefits of hypochlorous acid. Journal of Wound Care Published Online:5 Oct 2020https://www.karger.com/Article/Abstract/481545
4. Gold MH, Andriessen A, Bhatia AC, Bitter P Jr, Chilukuri S, Cohen JL, Robb CW. Topical stabilized hypochlorous acid: The future gold standard for wound care and scar management in dermatologic and plastic surgery procedures. J Cosmet Dermatol. 2020 Feb;19(2):270-277. https://pubmed.ncbi.nlm.nih.gov/31904191/
5. Prokopowicz ZM, Arce F, Biedroń R, Chiang CL, Ciszek M, Katz DR, Nowakowska M, Zapotoczny S, Marcinkiewicz J, Chain BM. Hypochlorous acid: a natural adjuvant that facilitates antigen processing, cross-priming, and the induction of adaptive immunity. J Immunol. 2010 Jan 15;184(2):824-35. https://pubmed.ncbi.nlm.nih.gov/20018624/
6. Pullar JM, Vissers MC, Winterbourn CC. Living with a killer: the effects of hypochlorous acid on mammalian cells. IUBMB Life. 2000 Oct-Nov;50(4-5):259-66. https://pubmed.ncbi.nlm.nih.gov/11327319/
7. Robson MC. Advancing the science of wound bed preparation for chronic wounds. Ostomy Wound Manag. 2012;58(12):2–3. https://www.o-wm.com/article/pearls-practice-advancing-science-wound-bed-preparation-chronic-wounds
8. Sakarya S, Gunay N, Karakulak M, Ozturk B, Ertugrul B. Hypochlorous acid: an ideal wound care agent with powerful microbicidal, antibiofilm, and wound healing potency. Wounds 2014;26(12):342–350. https://pubmed.ncbi.nlm.nih.gov/25785777/
9. Robson MC, Payne WG, Ko F, Mentis M, Donati G, Shafii SM, Culverhouse S, Wang L, Khosrovi B, Najafi R, Cooper DM, Bassiri M. Hypochlorous Acid as a Potential Wound Care Agent: Part II. Stabilized Hypochlorous Acid: Its Role in Decreasing Tissue Bacterial Bioburden and Overcoming the Inhibition of Infection on Wound Healing. J Burns Wounds. 2007 Apr 11;6:e6. https://pubmed.ncbi.nlm.nih.gov/17492051/<br/><br/>
<p class="MsoNormal" style="margin: 0in 0in 8pt; line-height: 15.693333625793457px; font-size: 11pt; font-family: Calibri, sans-serif; caret-color: #000000; color: #000000; font-style: normal; font-variant-caps: normal; font-weight: normal; letter-spacing: normal; orphans: auto; text-align: start; text-indent: 0px; text-transform: none; white-space: normal; widows: auto; word-spacing: 0px; -webkit-text-size-adjust: auto; -webkit-text-stroke-width: 0px; text-decoration: none;"><span style="font-size: 14pt; line-height: 19.97333335876465px;">We present a quantitative view of our extent of adoption in a 60-day period, via retrospective chart review. We present 21 surgical patients, their wound etiologies, and wound closure times. We reviewed our EMR charts manually/electronically to obtain the extent of cleanser usage to augment our plastic surgery practice. In addition, we present several illustrative cases where visual images show the ability of the cleanser to eliminate visible slough/necrotic tissue.</span></p>
</div><br/><br/><b>Results</b>: <div>
<p class="MsoNormal" style="margin: 0in 0in 8pt; line-height: 15.693333625793457px; font-size: 11pt; font-family: Calibri, sans-serif; caret-color: #000000; color: #000000; font-style: normal; font-variant-caps: normal; font-weight: normal; letter-spacing: normal; orphans: auto; text-align: start; text-indent: 0px; text-transform: none; white-space: normal; widows: auto; word-spacing: 0px; -webkit-text-size-adjust: auto; -webkit-text-stroke-width: 0px; text-decoration: none;"><span style="font-size: 14pt; line-height: 19.97333335876465px; color: black;">There were zero postoperative infections. One patient with hypertension had a postoperative hematoma. Skin graft take was 100% for the foot wound skin grafts. Skin graft take was 90% for the pelvic NSTI patient, who had flap tip ischemic loss of about 5% of the flap after ER transfer for pulmonary complications. Other patients all healed uneventfully within the standard accepted postoperative time periods. The calciphylaxis patient achieved 40% granulation of his infected wounds within 3 weeks postoperative, and he had significant pain relief. However, his renal failure progressed and he elected to transition to hospice.</span></p>
</div><br/><br/><b>Discussion</b>: <div>
<p class="MsoNormal" style="margin: 0in 0in 8pt; line-height: 15.693333625793457px; font-size: 11pt; font-family: Calibri, sans-serif; caret-color: #000000; color: #000000; font-style: normal; font-variant-caps: normal; font-weight: normal; letter-spacing: normal; orphans: auto; text-align: start; text-indent: 0px; text-transform: none; white-space: normal; widows: auto; word-spacing: 0px; -webkit-text-size-adjust: auto; -webkit-text-stroke-width: 0px; text-decoration: none;"><span style="font-size: 14pt; line-height: 19.97333335876465px;">We have used evidence-based guidelines to guide our wound bed cleansing and preparation practice. Clinical and preclinical published data indicate that the safety and efficacy of the pHA based cleanser is high. Our high adoption rate is illustrated in the data. Wound bed preparation is based on wound visual inspection, sharp excisional debridement, occasional wound cultures, and irrigation and cleansing. We have used these techniques to prove, via the illustrative cases, that the use of pHA is a sound and safe way to achieve wound healing goals. </span></p>
</div><br/><br/><b>Trademarked Items</b>: <br/><br/><b>References</b>: 1. Armstrong DG, Bohn G, Glat P, Kavros SJ, Kirsner R, Snyder R, Tettelbach W.Armstrong DG, et al. Expert Recommendations for the Use of Hypochlorous Solution: Science and Clinical Application. Ostomy Wound Management 2015 May;61(5): S2-S19. https://pubmed.ncbi.nlm.nih.gov/28692424/
2. Block, Michael S, and Brian G Rowan. “Hypochlorous Acid: A Review.” Journal of Oral and Maxillofacial Surgery: official journal of the American Association of Oral and Maxillofacial Surgeons vol. 78,9 (2020): 1461-1466. https://europepmc.org/article/med/32653307
3. Dissemond J. Wound Cleansing: benefits of hypochlorous acid. Journal of Wound Care Published Online:5 Oct 2020https://www.karger.com/Article/Abstract/481545
4. Gold MH, Andriessen A, Bhatia AC, Bitter P Jr, Chilukuri S, Cohen JL, Robb CW. Topical stabilized hypochlorous acid: The future gold standard for wound care and scar management in dermatologic and plastic surgery procedures. J Cosmet Dermatol. 2020 Feb;19(2):270-277. https://pubmed.ncbi.nlm.nih.gov/31904191/
5. Prokopowicz ZM, Arce F, Biedroń R, Chiang CL, Ciszek M, Katz DR, Nowakowska M, Zapotoczny S, Marcinkiewicz J, Chain BM. Hypochlorous acid: a natural adjuvant that facilitates antigen processing, cross-priming, and the induction of adaptive immunity. J Immunol. 2010 Jan 15;184(2):824-35. https://pubmed.ncbi.nlm.nih.gov/20018624/
6. Pullar JM, Vissers MC, Winterbourn CC. Living with a killer: the effects of hypochlorous acid on mammalian cells. IUBMB Life. 2000 Oct-Nov;50(4-5):259-66. https://pubmed.ncbi.nlm.nih.gov/11327319/
7. Robson MC. Advancing the science of wound bed preparation for chronic wounds. Ostomy Wound Manag. 2012;58(12):2–3. https://www.o-wm.com/article/pearls-practice-advancing-science-wound-bed-preparation-chronic-wounds
8. Sakarya S, Gunay N, Karakulak M, Ozturk B, Ertugrul B. Hypochlorous acid: an ideal wound care agent with powerful microbicidal, antibiofilm, and wound healing potency. Wounds 2014;26(12):342–350. https://pubmed.ncbi.nlm.nih.gov/25785777/
9. Robson MC, Payne WG, Ko F, Mentis M, Donati G, Shafii SM, Culverhouse S, Wang L, Khosrovi B, Najafi R, Cooper DM, Bassiri M. Hypochlorous Acid as a Potential Wound Care Agent: Part II. Stabilized Hypochlorous Acid: Its Role in Decreasing Tissue Bacterial Bioburden and Overcoming the Inhibition of Infection on Wound Healing. J Burns Wounds. 2007 Apr 11;6:e6. https://pubmed.ncbi.nlm.nih.gov/17492051/<br/><br/>

.png)