Back
Case Series/Study
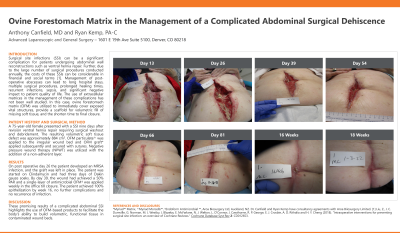
(CS-018) Ovine Forestomach Matrix in the Management of Complicated Abdominal Surgical Dehiscence
Co-Author(s):
Ryan Kemp, PA-C
<b>Introduction</b>: <p class="MsoNormal"><span lang="EN-GB">Surgical site infections (SSI) can be a significant complication for patients undergoing abdominal wall reconstructions such as ventral hernia repair</span><span lang="EN-GB" style="mso-ascii-font-family: Calibri; mso-ascii-theme-font: minor-latin; mso-hansi-font-family: Calibri; mso-hansi-theme-font: minor-latin; mso-bidi-font-family: Calibri; mso-bidi-theme-font: minor-latin;">. <span style="color: #212121; background: white;">Further, due to the large number of such procedure performed annually, costs of these SSIs can be considerable financial and social burden</span></span><span lang="EN-GB" style="mso-ascii-font-family: Calibri; mso-ascii-theme-font: minor-latin; mso-hansi-font-family: Calibri; mso-hansi-theme-font: minor-latin; mso-bidi-font-family: Calibri; mso-bidi-theme-font: minor-latin; color: #212121; background: white;"><span style="mso-no-proof: yes;">(Liu, Dumville et al. 2018)</span></span><span lang="EN-GB" style="mso-ascii-font-family: Calibri; mso-ascii-theme-font: minor-latin; mso-hansi-font-family: Calibri; mso-hansi-theme-font: minor-latin; mso-bidi-font-family: Calibri; mso-bidi-theme-font: minor-latin; color: #212121; background: white;">. SSIs can lead to long hospital stays, multiple surgical procedures, prolonged healing times, recurrent infections/sepsis. Use of ECMs in the management of SSIs has not been well-studied. In this case, Ovine Forestomach Matrix (OFM) was utilized to immediately cover exposed vital structures,\</span><span lang="EN-GB"> scaffold volumetric fill of soft tissue, and shorten time to final closure.</span></p><br/><br/><b>Methods</b>: <p class="MsoNormal"><span lang="EN-GB">A 75-year-old female presented with SSI nine days after ventral hernia repair. The SSI required hospital admission and surgical washout with debridement. Methicillin-resistant staphylococcus aureus (MRSA) was the isolated pathogen and resulting volumetric soft tissue defect measured approximately 884 cm<sup>3</sup>. OFM particulate^ was applied to the irregular wound bed, followed by application of OFM graft* which was secured with sutures. Once the wound volume was reduced to 50%, single-layer antimicrobial OFM</span><span lang="EN-GB" style="mso-bidi-font-size: 10.0pt;">†</span><span lang="EN-GB"> was then applied weekly at the bedside. Primary endpoints were time to 50% reduction in wound volume and time to 100% epithelialization. Secondary endpoints included scar and skin quality.</span></p><br/><br/><b>Results</b>: <p class="MsoNormal"><span lang="EN-GB" style="color: #010205;">Following surgical application of OFM particulate^ and graft*, the patient was able to achieve 50% wound volume reduction as of 5 weeks and was able to achieve full closure at 16 weeks following weekly application of single-layer OFM<span lang="EN-GB" style="font-size: 11.0pt; mso-bidi-font-size: 10.0pt; font-family: 'Calibri',sans-serif; mso-fareast-font-family: Calibri; mso-fareast-theme-font: minor-latin; mso-ansi-language: EN-GB; mso-fareast-language: EN-GB; mso-bidi-language: AR-SA;">† at bedside which negated the need for split-thickness skin graft</span>. The patient had no further complications and no recurrence of infection management with OFM despite the contaminated operative field and the known presence of a challenging pathogen such as MRSA. The patient had satisfactory skin closure and cosmesis with noted soft tissue pliability and minimal fibrotic scarring of the healed soft tissue.</span></p><br/><br/><b>Discussion</b>: <p class="MsoNormal"><span lang="EN-GB" style="mso-bidi-font-size: 10.0pt;">Surgical site infections can be challenging surgical complications that can consequently lead to large contaminated soft tissue defects which can lead to further morbidity, sepsis, prolonged hospital stays, and poor patient quality of life. The promising results of this case report of abdominal SSI complicated by MRSA highlights the use of OFM to build volumetric, functional granulation in contaminated wound beds affected by one of the more challenging pathogens. These preliminary data provides actionable clinical evidence that OFM can provide a cost-effective and clinically successful treatment tool for clinicians to treat large soft tissue defects caused by surgical site infections</span></p><br/><br/><b>Trademarked Items</b>: *Myriad™Matrix, Aroa Biosurgery Ltd, Auckland, NZ.
^Myriad Morcells™ Antimicrobial, Aroa Biosurgery Ltd, Auckland, NZ.
†Endoform Anti-Microbial ™, Aroa Biosurgery Ltd, Auckland, NZ.<br/><br/><b>References</b>: Liu, Z., J. C. Dumville, G. Norman, M. J. Westby, J. Blazeby, E. McFarlane, N. J. Welton, L. O'Connor, J. Cawthorne, R. P. George, E. J. Crosbie, A. D. Rithalia and H. Y. Cheng (2018). "Intraoperative interventions for preventing surgical site infection: an overview of Cochrane Reviews." Cochrane Database Syst Rev 2: CD012653.<br/><br/>
^Myriad Morcells™ Antimicrobial, Aroa Biosurgery Ltd, Auckland, NZ.
†Endoform Anti-Microbial ™, Aroa Biosurgery Ltd, Auckland, NZ.<br/><br/><b>References</b>: Liu, Z., J. C. Dumville, G. Norman, M. J. Westby, J. Blazeby, E. McFarlane, N. J. Welton, L. O'Connor, J. Cawthorne, R. P. George, E. J. Crosbie, A. D. Rithalia and H. Y. Cheng (2018). "Intraoperative interventions for preventing surgical site infection: an overview of Cochrane Reviews." Cochrane Database Syst Rev 2: CD012653.<br/><br/>

.png)