Back
Case Series/Study
(CS-059) Use of A Bioresorbable Silver Matrix on a Non-Healing TMA Site
Co-Author(s):
Jean Chen-Vitulli, DPM – Endocrine Associates of West Village; and Anastasios Manessis, MD – Endocrine Associates of West Village
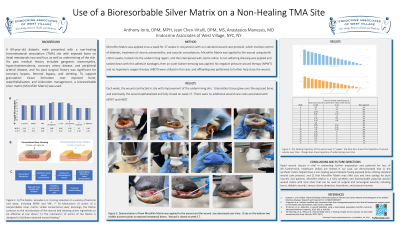
<b>Introduction</b>: <p class="MsoNormal">A 69-year-old diabetic male presented with a non-healing transmetatarsal amputation (TMA) site with exposed bone on distal metatarsals two and four, as well as undermining of the skin. His past medical history included gangrene, osteomyelitis, hypercholesterolemia, coronary artery disease, and peripheral arterial disease, and his past surgical history was significant for coronary bypass, femoral bypass, and stenting. To support granulation tissue formation over exposed bone, reepithelialization and bioburden management, a bioresorbable silver matrix (Microfilm Matrix) was used.</p><br/><br/><b>Methods</b>: <p class="MsoNormal">Microfilm Matrix was applied once a week for 17 weeks in conjunction with our standard wound care protocol, which involves control of diabetes, treatment of chronic osteomyelitis, and vascular consultations. Microfilm Matrix was applied to the wound using sterile cotton swabs, tucked into the undermining region, and then dampened with sterile saline. A non-adhering dressing was applied and tacked down with thin adhesive bandages, then an outer bolster dressing was applied. No negative pressure wound therapy (NPWT) and no hyperbaric oxygen therapy (HBOT) were utilized in this case, and offloading was performed to further help the wound close.</p><br/><br/><b>Results</b>: <p class="MsoNormal">Each week, the wound contracted in size with improvement of the undermining skin.<span style="mso-spacerun: yes;"> </span>Granulation tissue grew over the exposed bone, and eventually, the wound epithelialized and fully closed on week 17. There were no additional wound care costs associated with NPWT and HBOT.</p><br/><br/><b>Discussion</b>: <p class="MsoNormal">Rapid wound closure is vital in preventing further amputation and potential for loss of life. Furthermore, healthcare dollars are limited. In our case, we demonstrated that 1) the synthetic matrix helped close a non-healing wound despite having exposed bone utilizing standard wound care protocol, and 2) that Microfilm Matrix may offer cost and time savings for both insurers and patients. Microfilm Matrix is a fully synthetic and bioresorbable polyvinyl alcohol wound matrix with ionic silver that can be used on surgical and nonsurgical wounds, including burns, diabetic wounds, venous ulcers, abrasions, lacerations, and pressure injuries.</p><br/><br/><b>Trademarked Items</b>: <br/><br/><b>References</b>: 1) Sarah W. Manning, D. A. H., William R. Shillinglaw, Eric Crawford, Gaurav Pranami, Ankit Agarwal, Michael J.Schurr (2020). "Efficacy of a Bioresorbable Matrix in Healing Complex Chronic Wounds: An Open-LabelProspective Pilot Study." Wounds 32(11).
2) Chatelain, R. (2021). "The Efficacy of a Novel Silver-Containing Bioresorbable Microfilm Matrix in At-RiskSurgical Wounds: A Clinical Case Series." Wounds: a Compendium of Clinical Research and Practice 33(10):245-252.<br/><br/>
2) Chatelain, R. (2021). "The Efficacy of a Novel Silver-Containing Bioresorbable Microfilm Matrix in At-RiskSurgical Wounds: A Clinical Case Series." Wounds: a Compendium of Clinical Research and Practice 33(10):245-252.<br/><br/>

.png)