Back
Case Series/Study
(CS-037) Peripheral Nerve Reconstruction Using Placental Connective Tissue Matrix to Alleviate Phantom Limb Pain
Co-Author(s):
Suzanna Fitzpatrick, ACNP-BC, DNP – Senior Nurse Practitioner, Vascular Surgery, University of Maryland Medical Center; Khanjan Nagarsheth, MD – Vascular Surgery – University of Maryland Medical Center
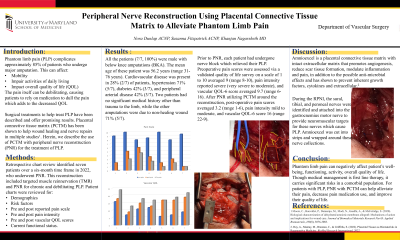
<b>Introduction</b>: <span style="font-size: 12.0pt; line-height: 107%; font-family: 'Times New Roman',serif; mso-fareast-font-family: 'Times New Roman'; color: black; mso-ansi-language: EN-US; mso-fareast-language: EN-US; mso-bidi-language: AR-SA;">Phantom limb pain (PLP)<span style="background: white;"> complicates approximately 85% of patients who undergo major amputation. This can affect mobility, impair ADLs, and overall quality of life. <span style="mso-spacerun: yes;"> </span></span>The pain itself can be debilitating, causing patients to rely on medication to dull the pain which adds to the decreased quality of life (QOL) for these patients. <span style="background: white;">Surgical treatments to help treat PLP have been described and offer promising results.</span> Placental connective tissue matrix (PCTM) has been shown to help wound healing and nerve repairs in multiple studies. Herein, we describe the use of PCTM with peripheral nerve reconstruction (PNR) for the treatment of PLP. </span><br/><br/><b>Methods</b>: <span style="font-size: 12.0pt; line-height: 107%; font-family: 'Times New Roman',serif; mso-fareast-font-family: 'Times New Roman'; color: black; background: white; mso-ansi-language: EN-US; mso-fareast-language: EN-US; mso-bidi-language: AR-SA;">A retrospective chart review identified seven patients over a six-month time frame in 2022, who underwent PNR. This reconstruction included targeted muscle reinnervation (TMR) and PNR for chronic and debilitating PLP. Patient charts were reviewed for demographics, risk factors, pre and post reported pain scale, pain intensity, and vascular quality of life (QOL) scores, in addition to current functional status.</span><br/><br/><b>Results</b>: <p class="MsoNormal" style="mso-margin-top-alt: auto; mso-margin-bottom-alt: auto; line-height: normal;"><span style="font-size: 12.0pt; font-family: 'Times New Roman',serif; mso-fareast-font-family: 'Times New Roman'; color: black; background: white;">All patients (7/7, 100%) were male with below knee amputations (BKA). Cardiovascular disease occurred in 28% (2/7), diabetes 42% (3/7), and PAD 42% (3/7). Two amputations were due to trauma, while the others had non-healing wounds 71% (5/7). </span></p>
<p class="MsoNormal" style="mso-margin-top-alt: auto; mso-margin-bottom-alt: auto; line-height: normal;"><span style="font-size: 12.0pt; font-family: 'Times New Roman',serif; mso-fareast-font-family: 'Times New Roman'; color: black; background: white;">Prior to PNR, patients underwent nerve block which relieved PLP. Preoperative pain scores and QOL were assessed via validated surveys. Averaged pain 9 (range 8-10), pain intensity severe (very severe to moderate), and QOL score 9.7 (range 6-16). After PNR utilizing PCTM around the reconstruction, post-operative pain averaged 3.2 (range 1-6), pain intensity mild to moderate, and QOL score 16 (range 22-9).</span></p><br/><br/><b>Discussion</b>: <span style="font-size: 12.0pt; line-height: 107%; font-family: 'Times New Roman',serif; mso-fareast-font-family: 'Times New Roman'; color: black; background: white; mso-ansi-language: EN-US; mso-fareast-language: EN-US; mso-bidi-language: AR-SA;">Phantom limb pain can negatively affect patient’s well-being, functioning, activity, overall quality of life. Though medical management is first line therapy, it carries significant risks in a comorbid population. For patients with PLP, PNR with PCTM can alleviate their pain, decrease pain medication use, and improve their quality of life. </span><br/><br/><b>Trademarked Items</b>: <br/><br/><b>References</b>: <br/><br/>
<p class="MsoNormal" style="mso-margin-top-alt: auto; mso-margin-bottom-alt: auto; line-height: normal;"><span style="font-size: 12.0pt; font-family: 'Times New Roman',serif; mso-fareast-font-family: 'Times New Roman'; color: black; background: white;">Prior to PNR, patients underwent nerve block which relieved PLP. Preoperative pain scores and QOL were assessed via validated surveys. Averaged pain 9 (range 8-10), pain intensity severe (very severe to moderate), and QOL score 9.7 (range 6-16). After PNR utilizing PCTM around the reconstruction, post-operative pain averaged 3.2 (range 1-6), pain intensity mild to moderate, and QOL score 16 (range 22-9).</span></p><br/><br/><b>Discussion</b>: <span style="font-size: 12.0pt; line-height: 107%; font-family: 'Times New Roman',serif; mso-fareast-font-family: 'Times New Roman'; color: black; background: white; mso-ansi-language: EN-US; mso-fareast-language: EN-US; mso-bidi-language: AR-SA;">Phantom limb pain can negatively affect patient’s well-being, functioning, activity, overall quality of life. Though medical management is first line therapy, it carries significant risks in a comorbid population. For patients with PLP, PNR with PCTM can alleviate their pain, decrease pain medication use, and improve their quality of life. </span><br/><br/><b>Trademarked Items</b>: <br/><br/><b>References</b>: <br/><br/>

.png)