Case Series/Study
(CS-106) Enteric Fistula Management using Pure Hypochlorous Acid Wound Cleanser
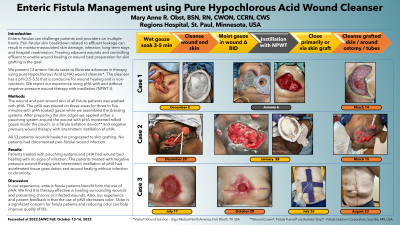
Enteric fistulas can challenge patients and providers on multiple fronts. Peri-fistular skin breakdown related to effluent leakage can result in moisture-associated skin damage, infection, long-term stays and hospital readmission. Treating adjacent wounds and controlling effluent to enable wound healing or wound bed preparation for skin grafting is the goal.
We present 13 enteric fistula cases to illustrate advances in therapy using pure Hypochlorous Acid (pHA) wound cleanser*. The cleanser has a pH (3.5-5.5) that is conducive for wound healing and is non-cytotoxic. We report our experience using pHA with and without negative pressure wound therapy with instillation (NPWT-i).
Methods:
The wound and peri-wound skin of all fistula patients was washed with pHA. The pHA was placed on these areas for three to five minutes with pHA soaked gauze while we assembled the dressing systems. After preparing the skin edges we applied either a pouching system around the wound with pHA moistened rolled gauze inside the pouch, or a fistula isolation device** and negative pressure wound therapy with intermittent instillation of pHA.
All 13 patients’ wounds healed or progressed to skin grafting. No patients had documented peri-fistular wound infection.
Results:
Patients treated with pouching systems and pHA had wound bed healing with no signs of infection. The patients treated with negative pressure wound therapy with intermittent instillation of pHA had accelerated tissue granulation and wound healing without infection or chronicity.
Discussion:
In our experience, enteric fistula patients benefit from the use of pHA. We find this therapy effective in healing surrounding wounds and preventing chronic or infected wounds. Also, our experience and patient feedback is that the use of pHA decreases odor. Odor is a significant concern for fistula patients and reducing odor can help improve quality of life.
Trademarked Items:
References: 1. Kim PJ, Attinger CE, Constantine T, et al. Negative pressure wound therapy with instillation: International consensus guidelines update. Int Wound J. 2020;17:174– 186.
2. Melphine M. Harriott, Nayan Bhindi, Salam Kassis, Blair Summitt, Galen Perdikis, Blair A. Wormer, Timothy M. Rankin, Christodoulos Kaoutzanis, Mario Samaha, Charles Stratton, Jonathan E. Schmitz. Comparative Antimicrobial Activity of Commercial Wound-Care Solutions on Bacterial and Fungal Biofilms, Ann Plast Surg. 83(4): 404–410, 2019.
3. White GC, “Handbook of Chlorination and alternative disinfectants.” 4th Edition, 1999, Wiley Interscience, p.215 – 219.
4. Hidalgo E, Bartolome R, Dominguez C. Cytotoxicity mechanisms of sodium hypochlorite in cultured human dermal fibroblasts and its bactericidal effectiveness. Chem Biol Interact. 2002 Mar 20;139(3):265-82.
5. Kozol RA, Gillies C, Elgebaly SA. Effects of sodium hypochlorite (Dakin's solution) on cells of the wound module. Arch Surg. 1988 Apr;123(4):420-3.
6. Gethin, Georgina. (2007). The significance of surface pH in chronic wounds. Wounds UK. 3 (3) 52-56.
7. Nagoba BS, Suryawanshi NM, Wadher B, Selkar S. Acidic environment and wound healing: a review, Wounds 2015;27(1):5-11.
8. Hiebert JM, Robson MC. The Immediate and Delayed Post-Debridement Effects on Tissue Bacterial Wound Counts of Hypochlorous Acid Versus Saline Irrigation in Chronic Wounds. Eplasty. 2016;16: e32. Published 2016 Dec 1.
9. Alberto CE, MD, Cardenas L, Cipolle M, Gallagher KE. Level 1 Trauma center experience utilizing negative pressure wound therapy with instillation: hypochlorous acid versus normal saline solution in complex or infected wounds. J Med. Sci. Clin. Res. 2020;8(6): 414-420
10. Sakarya S, Gunay N, Karakulak M, Ozturk B, Ertugrul B. Hypochlorous acid: an ideal wound care agent with powerful microbicidal, antibiofilm, and wound healing potency. Wounds 2014;26(12):342–350.
11. Armstrong DG, Bohn G, Glat P, Kavros SJ, Kirsner R, Snyder R, Tettelbach W.Armstrong DG, et al. Expert Recommendations for the Use of Hypochlorous Solution: Science and Clinical Application. Ostomy Wound Management 2015 May;61(5): S2-S19.
12. Robson MC. Treating chronic wounds with hypochlorous acid disrupts biofilm. Wound Prevention and Management 2020;66 (5):9-10.
13. Sauer K, Thatcher E, Northey R, Gutierrez AA. Neutral super-oxidised solutions are effective in killing P. aeruginosa biofilms. Biofouling 2009;25(1):45-54.
14. Day A, Alkhalil A, Carney BC, Hoffman HN, Moffatt LT, Shupp JW. Disruption of Biofilms and Neutralization of Bacteria Using Hypochlorous Acid Solution: An In Vivo and In Vitro Evaluation. Adv Skin Wound Care 2017 Dec;30(12):543-551.

.png)