Back
Case Series/Study
(CS-026) Steroids, Bioengineered Skin Substitute, and Transforming Powder Dressing: Combination Therapy for Pyoderma Gangrenosum
Co-Author(s):
Avi Hatami, MD; Brian Gillette, PhD; Scott Gorenstein, MD
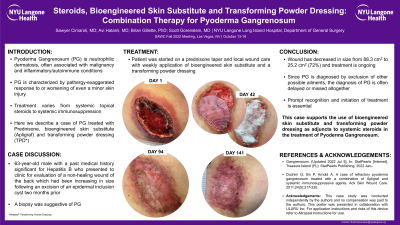
<b>Introduction</b>: <div><span class="normaltextrun">Pyoderma Gangrenosum (PG) is neutrophilic dermatosis which is often associated with malignancy and inflammatory/autoimmune conditions. The hallmark of PG is pathergy or an exaggerated response to or worsening of even a minor skin injury. Treatment depends on disease severity and varies from topical steroids to systemic immunosuppression. The local wound care for PG is not well established and depends on provider experience and preference. </span><span class="eop">Here we present a case of Pyoderma Gangrenosum treated with Prednisone, </span><span class="normaltextrun">bioengineered skin substitute, </span><span class="normaltextrun">and transforming powder dressing.<br /><br />Would not allow submission without 400 words.Would not allow submission without 400 words. Please disregard these additional words.<br /></span></div><br/><br/><b>Methods</b>: <div><span class="normaltextrun" style="caret-color: #000000; color: #000000; font-style: normal; font-variant-caps: normal; font-weight: 400; letter-spacing: normal; orphans: auto; text-align: start; text-indent: 0px; text-transform: none; white-space: normal; widows: auto; word-spacing: 0px; -webkit-text-size-adjust: auto; -webkit-text-stroke-width: 0px; text-decoration: none;"><span style="font-size: 11pt; font-family: Calibri, sans-serif;">This is a retrospective case review of a 63-year-old male with a past medical history significant for Hepatitis B who presented for evaluation of a non-healing wound of the back which had been increasing in size following an excision of an epidermal inclusion cyst two months prior. The patient had reported increased pain and purulent drainage from the wound. The selected treatment protocol included use of steroids, application of a <a>bioengineered skin substitute and transforming powder dressing. The TPD was applied to the wound between skin substitute applications and was placed on top of the skin substitute to secure it. </a></span></span></div>
<div> <br /><br /></div><br/><br/><b>Results</b>: <div>
<p class="paragraph"><span class="normaltextrun">On examination, the wound was moist with a necrotic base, undermining, and peri-wound edema. The patient was admitted for IV antibiotics and debridement of devitalized tissue. A biopsy was obtained during the procedure which was concerning for Pyoderma Gangrenosum (suppurative granulomatous dermatitis with abscess with stains negative for microorganisms). Post operatively, the patient was started on a Prednisone taper and the wound was treated with weekly application of bioengineered skin substitute, and transforming powder dressing. The patient is still undergoing treatment; however, the wound has decreased in size from 88.3cm<sup>2</sup> to 25.2cm<sup>2</sup>.<br /><br />Would not allow submission without 400 words. Disregard.<br /></span></p>
</div><br/><br/><b>Discussion</b>: <div>
<p class="paragraph"><span class="normaltextrun">Pyoderma Gangrenosum is frequently missed diagnosed as infection or other cause for delayed wound healing. PG is a typically made via diagnosis of exclusion; the diagnosis is often delayed or missed all together. Prompt recognition and initiation of systemic steroids with local wound care is essential to prevent disease progression. Often patients undergo multiple debridments which perpetuate the disease process. This case presents the use of bioengineered skin substitute and transforming powder dressing as safe, effective adjuncts to systemic steroids in the treatment of Pyoderma Gangrenosum.<br /><br /><br />Would not allow submission without 400 words. Would not allow submission without 400 words. </span></p>
</div><br/><br/><b>Trademarked Items</b>: Altrazeal and Apligraf<br/><br/><b>References</b>: <br/><br/>
<div> <br /><br /></div><br/><br/><b>Results</b>: <div>
<p class="paragraph"><span class="normaltextrun">On examination, the wound was moist with a necrotic base, undermining, and peri-wound edema. The patient was admitted for IV antibiotics and debridement of devitalized tissue. A biopsy was obtained during the procedure which was concerning for Pyoderma Gangrenosum (suppurative granulomatous dermatitis with abscess with stains negative for microorganisms). Post operatively, the patient was started on a Prednisone taper and the wound was treated with weekly application of bioengineered skin substitute, and transforming powder dressing. The patient is still undergoing treatment; however, the wound has decreased in size from 88.3cm<sup>2</sup> to 25.2cm<sup>2</sup>.<br /><br />Would not allow submission without 400 words. Disregard.<br /></span></p>
</div><br/><br/><b>Discussion</b>: <div>
<p class="paragraph"><span class="normaltextrun">Pyoderma Gangrenosum is frequently missed diagnosed as infection or other cause for delayed wound healing. PG is a typically made via diagnosis of exclusion; the diagnosis is often delayed or missed all together. Prompt recognition and initiation of systemic steroids with local wound care is essential to prevent disease progression. Often patients undergo multiple debridments which perpetuate the disease process. This case presents the use of bioengineered skin substitute and transforming powder dressing as safe, effective adjuncts to systemic steroids in the treatment of Pyoderma Gangrenosum.<br /><br /><br />Would not allow submission without 400 words. Would not allow submission without 400 words. </span></p>
</div><br/><br/><b>Trademarked Items</b>: Altrazeal and Apligraf<br/><br/><b>References</b>: <br/><br/>

.png)