Back
Case Series/Study
(CS-025) The Utility of Transforming Powder Dressing in the Treatment of Various Wound Types: A Case Series
Co-Author(s):
James Daniels, MD; Danilo Lozada, MS; Brian Gillette, PhD; Scott Gorenstein, MD
<b>Introduction</b>: <div>
<p class="MsoNormal" style="margin: 0in 0in 0.0001pt; font-size: medium; font-family: Calibri, sans-serif; caret-color: #000000; color: #000000; font-style: normal; font-variant-caps: normal; font-weight: 400; letter-spacing: normal; orphans: auto; text-align: start; text-indent: 0px; text-transform: none; white-space: normal; widows: auto; word-spacing: 0px; -webkit-text-size-adjust: auto; -webkit-text-stroke-width: 0px; text-decoration: none;"><span style="font-family: 'Times New Roman', serif; color: black;">Over 8 million people a year receive wound treatment in the United States.</span> <span style="font-family: 'Times New Roman', serif; color: black;">Increasing health care costs, limited healthcare resources, an aging population, and life-style related diseases make wound management a growing clinical, social, and economic burden, indicating a vital need for a more effective wound management solutions. </span><span style="font-family: 'Times New Roman', serif;">A novel, <span style="color: black;">biocompatible polymer-based transforming powder dressing (TPD), which transforms in-situ to a shape-retentive wound matrix upon hydration, has demonstrated positive results in independent case studies in individual wounds of various etiologies. </span>This case series was conducted to examine the effect of TPD in the treatment of various acute and chronic wounds.</span></p>
</div><br/><br/><b>Methods</b>: <div>
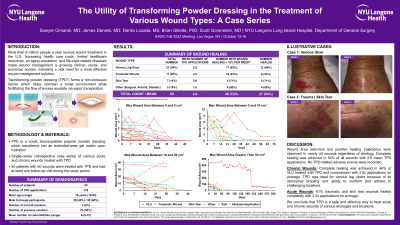
<p class="MsoNormal" style="margin: 0in 0in 12pt; font-size: medium; font-family: Calibri, sans-serif; caret-color: #000000; color: #000000; font-style: normal; font-variant-caps: normal; font-weight: 400; letter-spacing: normal; orphans: auto; text-align: start; text-indent: 0px; text-transform: none; white-space: normal; widows: auto; word-spacing: 0px; -webkit-text-size-adjust: auto; -webkit-text-stroke-width: 0px; text-decoration: none;"><span style="font-family: 'Times New Roman', serif; color: black;">This was an IRB-approved single-center retrospective case series of </span><span style="font-family: 'Times New Roman', serif;">various acute and chronic wounds treated with<span style="color: black;"> TPD over a period of two years. Wound etiology, location, number of applications, change in wound surface area, and comorbidities were evaluated. Wounds were followed from the first TPD application up to one month after the last TPD application or until the wound healed or the patient was lost to follow up, whichever came first. </span></span></p>
</div><br/><br/><b>Results</b>: <div>
<p class="MsoNormal" style="margin: 0in 0in 0.0001pt; font-size: medium; font-family: Calibri, sans-serif; caret-color: #000000; color: #000000; font-style: normal; font-variant-caps: normal; font-weight: 400; letter-spacing: normal; orphans: auto; text-align: start; text-indent: 0px; text-transform: none; white-space: normal; widows: auto; word-spacing: 0px; -webkit-text-size-adjust: auto; -webkit-text-stroke-width: 0px; text-decoration: none;"><span style="font-family: 'Times New Roman', serif; color: black;">We identified 50 patients that were treated with TPD</span><span style="font-family: 'Times New Roman', serif;"> and had at least one follow-up visit during the study period. The majority of wounds treated with TPD were venous leg ulcers (n=27), traumatic wounds (n=11), and skin tears (n=7). The majority of patients were treated over a period of up to 40 days (36/50, 72%). Normal wound healing ( >10% per week) was observed in most patients (36/50, 72%). Complete healing during the study period was observed in 43% of venous leg ulcers, 55% of traumatic wounds, and 71% of skin tears. No adverse effects of TPD administration were observed.</span></p>
</div><br/><br/><b>Discussion</b>: <div>
<p class="MsoNormal" style="margin: 0in 0in 0.0001pt; font-size: medium; font-family: Calibri, sans-serif; caret-color: #000000; color: #000000; font-style: normal; font-variant-caps: normal; font-weight: 400; letter-spacing: normal; orphans: auto; text-align: start; text-indent: 0px; text-transform: none; white-space: normal; widows: auto; word-spacing: 0px; -webkit-text-size-adjust: auto; -webkit-text-stroke-width: 0px; text-decoration: none;"><span style="font-family: 'Times New Roman', serif; color: black;">After treatment with TPD, we saw significant reductions in wound area of nearly all wounds, regardless of etiology. We conclude that TPD </span><span style="font-family: 'Times New Roman', serif;">was a safe and effective way to treat wounds of various etiologies and locations. </span></p>
</div><br/><br/><b>Trademarked Items</b>: Altrazeal Transforming Powder Dressing<br/><br/><b>References</b>: <br/><br/>
<p class="MsoNormal" style="margin: 0in 0in 0.0001pt; font-size: medium; font-family: Calibri, sans-serif; caret-color: #000000; color: #000000; font-style: normal; font-variant-caps: normal; font-weight: 400; letter-spacing: normal; orphans: auto; text-align: start; text-indent: 0px; text-transform: none; white-space: normal; widows: auto; word-spacing: 0px; -webkit-text-size-adjust: auto; -webkit-text-stroke-width: 0px; text-decoration: none;"><span style="font-family: 'Times New Roman', serif; color: black;">Over 8 million people a year receive wound treatment in the United States.</span> <span style="font-family: 'Times New Roman', serif; color: black;">Increasing health care costs, limited healthcare resources, an aging population, and life-style related diseases make wound management a growing clinical, social, and economic burden, indicating a vital need for a more effective wound management solutions. </span><span style="font-family: 'Times New Roman', serif;">A novel, <span style="color: black;">biocompatible polymer-based transforming powder dressing (TPD), which transforms in-situ to a shape-retentive wound matrix upon hydration, has demonstrated positive results in independent case studies in individual wounds of various etiologies. </span>This case series was conducted to examine the effect of TPD in the treatment of various acute and chronic wounds.</span></p>
</div><br/><br/><b>Methods</b>: <div>
<p class="MsoNormal" style="margin: 0in 0in 12pt; font-size: medium; font-family: Calibri, sans-serif; caret-color: #000000; color: #000000; font-style: normal; font-variant-caps: normal; font-weight: 400; letter-spacing: normal; orphans: auto; text-align: start; text-indent: 0px; text-transform: none; white-space: normal; widows: auto; word-spacing: 0px; -webkit-text-size-adjust: auto; -webkit-text-stroke-width: 0px; text-decoration: none;"><span style="font-family: 'Times New Roman', serif; color: black;">This was an IRB-approved single-center retrospective case series of </span><span style="font-family: 'Times New Roman', serif;">various acute and chronic wounds treated with<span style="color: black;"> TPD over a period of two years. Wound etiology, location, number of applications, change in wound surface area, and comorbidities were evaluated. Wounds were followed from the first TPD application up to one month after the last TPD application or until the wound healed or the patient was lost to follow up, whichever came first. </span></span></p>
</div><br/><br/><b>Results</b>: <div>
<p class="MsoNormal" style="margin: 0in 0in 0.0001pt; font-size: medium; font-family: Calibri, sans-serif; caret-color: #000000; color: #000000; font-style: normal; font-variant-caps: normal; font-weight: 400; letter-spacing: normal; orphans: auto; text-align: start; text-indent: 0px; text-transform: none; white-space: normal; widows: auto; word-spacing: 0px; -webkit-text-size-adjust: auto; -webkit-text-stroke-width: 0px; text-decoration: none;"><span style="font-family: 'Times New Roman', serif; color: black;">We identified 50 patients that were treated with TPD</span><span style="font-family: 'Times New Roman', serif;"> and had at least one follow-up visit during the study period. The majority of wounds treated with TPD were venous leg ulcers (n=27), traumatic wounds (n=11), and skin tears (n=7). The majority of patients were treated over a period of up to 40 days (36/50, 72%). Normal wound healing ( >10% per week) was observed in most patients (36/50, 72%). Complete healing during the study period was observed in 43% of venous leg ulcers, 55% of traumatic wounds, and 71% of skin tears. No adverse effects of TPD administration were observed.</span></p>
</div><br/><br/><b>Discussion</b>: <div>
<p class="MsoNormal" style="margin: 0in 0in 0.0001pt; font-size: medium; font-family: Calibri, sans-serif; caret-color: #000000; color: #000000; font-style: normal; font-variant-caps: normal; font-weight: 400; letter-spacing: normal; orphans: auto; text-align: start; text-indent: 0px; text-transform: none; white-space: normal; widows: auto; word-spacing: 0px; -webkit-text-size-adjust: auto; -webkit-text-stroke-width: 0px; text-decoration: none;"><span style="font-family: 'Times New Roman', serif; color: black;">After treatment with TPD, we saw significant reductions in wound area of nearly all wounds, regardless of etiology. We conclude that TPD </span><span style="font-family: 'Times New Roman', serif;">was a safe and effective way to treat wounds of various etiologies and locations. </span></p>
</div><br/><br/><b>Trademarked Items</b>: Altrazeal Transforming Powder Dressing<br/><br/><b>References</b>: <br/><br/>

.png)