Back
Case Series/Study
(CS-080) Utilization of Rich Omega3 Fatty Acid Fish Skin in Healing Soft Tissue Deficits in the Presence of Infection
Co-Author(s):
Richard Bruno, D.P.M. – Assistant Director, Eastern Virginia Medical School Podiatric Residency Program; Brandon Blanken, D.P.M. – Eastern Virginia Medical School Podiatric Residency Program; Adam Bhatti, D.P.M. – Eastern Virginia Medical School Podiatric Residency Program; Marisa Mosier, D.P.M. – Eastern Virginia Medical School Podiatric Residency Program
Introduction: Osteomyelitis, abscesses, and Charcot Neuroarthropathy have the predilection to leave substantial soft tissue deficits for many patients. The diabetic population are highly predisposed to these pathologies and often undergo surgical procedures to eradicate and restore function. In the latter portion of staged procedures, often times these patients are faced with the complicated task of achieving full wound healing. Thus, the aim of this study is to exhibit the success of rich, omega-3 fatty acid fish skin xenografts, such as Kerecis® Omega3 Wound in healing detrimental wounds in compromised conditions.
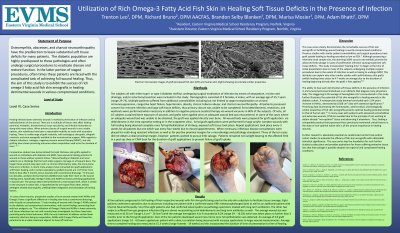
Methods: A total of ten patients demonstrating advanced combordities were grafted using Kerecis® Omega3 Wound either serially, or a one time application. Grafts were applied either in the outpatient setting after wound bed preparation or in the operating room following formal surgical debridement. All patients included in the study exhibited an infectious or inflammatory process. Electronic medical records were reviewed and included all patients possessing at least a one year follow up. Additional factors implemented during the healing course included the presence of surgical procedures, negative wound pressure therapy, antibiotics, and off-loading.
Results: All ten subjects underwent grafting with fish skin substitute with no graft rejections or complications occurring. Graft incorporation was confirmed and documented in the outpatient setting with substantial decrease in wound size occurring. All wounds remained healed at time of most recent follow-up which was recorded at a minimum of one year. Graft incorporation was confirmed and as of most recent follow-up, no wounds have reoccured. Of note, the average A1c of all subjects was greater than 9.0% and certain subjects healed deficits in the presence of confirmed osteomyelitis via radiography and/or biopsy, in those wanting to pursue limb salvage.
Discussion: The homogenous microbiology behind the Kerecis® Omega3 Wound skin substitute used exhibits many similar qualities to that of human skin, while also providing enhanced growth factors, hemostasis, and antimicrobial properties. The success demonstrated in its healing efficacy shows great potential in wound care in the most complicated healing environments while enhancing return to function. With the inherent ability to also prevent donor site morbidity and its remarkable success rate, this data suggests continued use of Kerecis® Omega3 Wound as a viable option in healing complicated wounds.
Trademarked Items: Kerecis® Omega3 Wound
References: Gordon, A. J., Alfonso, A. R., Nicholson, J., & Chiu, E. S. (2019). Evidence for healing diabetic foot ulcers with biologic skin substitutes: a systematic review and meta-analysis. Annals of plastic surgery, 83(4S), S31-S44.
Holl, J., Kowalewski, C., Zimek, Z., Fiedor, P., Kaminski, A., Oldak, T., ... & Eljaszewicz, A. (2021). Chronic diabetic wounds and their treatment with skin substitutes. Cells, 10(3), 655.
Kerecis® Omega3 Wound Official Website
Naz, I., Walters, E. T., Janhofer, D. E., Penzler, M. M., Tefera, E. A., Evans, K. K., ... & Kim, P. J. (2019). Outcomes of Split-thickness Skin Grafting for Foot and Ankle Wounds in Patients With Peripheral Arterial Disease. Wounds: a Compendium of Clinical Research and Practice, 31(11), 272-278.
Ramanujam, C. L., & Zgonis, T. (2012). Surgical soft tissue closure of severe diabetic foot infections: a combination of biologics, negative pressure wound therapy, and skin grafting. Clinics in podiatric medicine and surgery, 29(1), 143-146.
Rose, J. F., Giovinco, N., Mills, J. L., Najafi, B., Pappalardo, J., & Armstrong, D. G. (2014). Split-thickness skin grafting the high-risk diabetic foot. Journal of vascular surgery, 59(6), 1657-1663.
Roukis, T. S., & Zgonis, T. (2005). Skin grafting techniques for soft-tissue coverage of diabetic foot and ankle wounds. Journal of wound care, 14(4), 173-176.
Sanniec, K., Nguyen, T., van Asten, S., Fontaine, J. L., & Lavery, L. A. (2017). Split-thickness skin grafts to the foot and ankle of diabetic patients. Journal of the American Podiatric Medical Association, 107(5), 365-368.
Santema, T. K., Poyck, P. P., & Ubbink, D. T. (2016). Systematic review and meta‐analysis of skin substitutes in the treatment of diabetic foot ulcers: highlights of a Cochrane systematic review. Wound Repair and Regeneration, 24(4), 737-744.
Methods: A total of ten patients demonstrating advanced combordities were grafted using Kerecis® Omega3 Wound either serially, or a one time application. Grafts were applied either in the outpatient setting after wound bed preparation or in the operating room following formal surgical debridement. All patients included in the study exhibited an infectious or inflammatory process. Electronic medical records were reviewed and included all patients possessing at least a one year follow up. Additional factors implemented during the healing course included the presence of surgical procedures, negative wound pressure therapy, antibiotics, and off-loading.
Results: All ten subjects underwent grafting with fish skin substitute with no graft rejections or complications occurring. Graft incorporation was confirmed and documented in the outpatient setting with substantial decrease in wound size occurring. All wounds remained healed at time of most recent follow-up which was recorded at a minimum of one year. Graft incorporation was confirmed and as of most recent follow-up, no wounds have reoccured. Of note, the average A1c of all subjects was greater than 9.0% and certain subjects healed deficits in the presence of confirmed osteomyelitis via radiography and/or biopsy, in those wanting to pursue limb salvage.
Discussion: The homogenous microbiology behind the Kerecis® Omega3 Wound skin substitute used exhibits many similar qualities to that of human skin, while also providing enhanced growth factors, hemostasis, and antimicrobial properties. The success demonstrated in its healing efficacy shows great potential in wound care in the most complicated healing environments while enhancing return to function. With the inherent ability to also prevent donor site morbidity and its remarkable success rate, this data suggests continued use of Kerecis® Omega3 Wound as a viable option in healing complicated wounds.
Trademarked Items: Kerecis® Omega3 Wound
References: Gordon, A. J., Alfonso, A. R., Nicholson, J., & Chiu, E. S. (2019). Evidence for healing diabetic foot ulcers with biologic skin substitutes: a systematic review and meta-analysis. Annals of plastic surgery, 83(4S), S31-S44.
Holl, J., Kowalewski, C., Zimek, Z., Fiedor, P., Kaminski, A., Oldak, T., ... & Eljaszewicz, A. (2021). Chronic diabetic wounds and their treatment with skin substitutes. Cells, 10(3), 655.
Kerecis® Omega3 Wound Official Website
Naz, I., Walters, E. T., Janhofer, D. E., Penzler, M. M., Tefera, E. A., Evans, K. K., ... & Kim, P. J. (2019). Outcomes of Split-thickness Skin Grafting for Foot and Ankle Wounds in Patients With Peripheral Arterial Disease. Wounds: a Compendium of Clinical Research and Practice, 31(11), 272-278.
Ramanujam, C. L., & Zgonis, T. (2012). Surgical soft tissue closure of severe diabetic foot infections: a combination of biologics, negative pressure wound therapy, and skin grafting. Clinics in podiatric medicine and surgery, 29(1), 143-146.
Rose, J. F., Giovinco, N., Mills, J. L., Najafi, B., Pappalardo, J., & Armstrong, D. G. (2014). Split-thickness skin grafting the high-risk diabetic foot. Journal of vascular surgery, 59(6), 1657-1663.
Roukis, T. S., & Zgonis, T. (2005). Skin grafting techniques for soft-tissue coverage of diabetic foot and ankle wounds. Journal of wound care, 14(4), 173-176.
Sanniec, K., Nguyen, T., van Asten, S., Fontaine, J. L., & Lavery, L. A. (2017). Split-thickness skin grafts to the foot and ankle of diabetic patients. Journal of the American Podiatric Medical Association, 107(5), 365-368.
Santema, T. K., Poyck, P. P., & Ubbink, D. T. (2016). Systematic review and meta‐analysis of skin substitutes in the treatment of diabetic foot ulcers: highlights of a Cochrane systematic review. Wound Repair and Regeneration, 24(4), 737-744.

.png)