Back
Purpose: Airborne SARS-CoV-2 infection can be tackled by antiviral drug targeted delivery to infected cells of upper airway. Timely antiviral treatment at symptom onset would stop virus spreading to lung and other organs, sparing severe disease. Chloroquine diphosphate (CQ) and favipiravir (FPV) can be repurposed to such objective. Thus, we studied the formulation of CQ and FPV microparticles for in vitro deposition into the upper airway epithelia as aerosol (by nasal powder breath-inspiration in vivo).
Methods: CQ and FPV were independently transformed into microparticles by spray drying from aqueous solutions [1]. 1% (w/w) sodium stearate was added to the composition in both cases (CQ-MPs, FPV-MPs). Additional CQ formulations comprised a zinc salt as drug adjuvant (CQ-binary) and lactoferrin as mucoadhesive agent (CQ-ternary). Powders were characterized for size distribution, morphology, drug content, ex vivo transport across excised rabbit nasal mucosa. The amount of CQ and FPV accumulated in the epithelial cells was measured, also varying the contact time between formulation and mucosa. Powder respirability was preliminarily measured by Fast Screening Impactor, using the RS01® medium resistance dry powder inhaler at 60 L/min air flow rate. Finally, the inhibitory effect of CQ powders against SARS-CoV-2 was determined in vitro on Vero E6 cells. The cells were treated either applying drug after viral inoculum or pre-treating cells with drug before viral inoculum, then treating.
Results: For both APIs, spray drying process formed microparticles with median volume diameter (Dv,0.5) lower than 5 µm, with satisfactory yields (50-85%). For CQ compositions, microparticle morphology was perfectly spherical and surface smooth, when CQ was spray-dried with Na stearate. Zn salt and Zn salt+lactoferrin changed such morphology to corrugated and wrinkled, highlighting a strong effect of the protein on microparticle formation during droplet drying [Fig. 1]. Drug content was according to the theoretical composition for both CQ and FPV, proving drug stability during process. Both APIs crossed quite extensively the rabbit nasal mucosa ex vivo. In detail, the 3.5-h application of an amount of spray-dried powder equivalent to 5 mg of CQ free base (+ 0.1 ml liquid to wet), led to CQ amounts transported per unit area shown in Table I. These amounts corresponded to 40%-63% of CQ initially loaded in the donor. Similarly, almost 60% of loaded FPV (7.5 mg) was found in the receptor compartment at 210 minutes. More interestingly, after extraction from the mucosa and quantification, we found that both APIs highly concentrated inside the mucosal tissue. For CQ, knowing mucosal surface and thickness, drug concentration levels in the tissue were calculated [Fig. 2]. With the ternary powder (CQ + zinc + lactoferrin), we determined that CQ concentrations in the mucosa were higher after shorter contact time between formulation and mucosa (15, 30 and 45 min), as it would happen in vivo [Fig. 3]. Similarly, FPV concentration in the tissue after 30 minutes was 7.4 ± 1.3 mM. With emitted doses >85%, the fine particle fraction (%) of the 3 chloroquine powders ranged from 32.4 ± 2.2% of CQ-binary to 44.4 ± 4.4% of CQ-MPs, likely due to the presence of Na stearate. Although the powder product is for nasal inspiration, a certain degree of respirability is favorable for extending the deposition to the upper airways, including larynx and trachea, where the virus also infects. Finally, when drug treatment in vitro was applied after virus inoculum (MOI 0.05 and 0.005), either once or for 3 consecutive times, the % inhibition of viral replication increased with CQ concentration (from 25 to 75 µM) for all compositions, although not linearly. Compared to one treatment only, three treatments post-infection made the greatest difference in terms of % inhibition, reaching close to 100% inhibition with 3 treatments at 50 µM CQ diphosphate. The powder composition did not substantially affect CQ inhibitory activity. Furthermore, at all CQ concentrations, the 2-hour pre-treatment of cells before virus inoculum, significantly increased the antiviral effect of the subsequent 1 or 3 treatments post-infection. In particular, pre-treatment led to % inhibition values about 3-4 folds or 1.5 folds as higher, respectively when one or three treatments post-infection were carried out.
Conclusion: The investigated spray-dried CQ and FPV microparticles possess the necessary quality attributes to be inspired via the nose and deposited on the upper airway mucosae. Their dissolution on target creates a saturated solution rapidly accumulating the drugs in the infected cells at concentrations of more than 3 orders those inhibiting virus replication in vitro. As nasal doses are much lower than those required if the drug is given systemically, the product’s safety profile is expected high. Thus, the product could be effectively used at first symptoms, even while waiting for the COVID-19 test result.
References: 1. PCT/EP2008/059110; WO 2010/003465 A2
Acknowledgements:This research was funded by part of the generous donations received during the 2021 Crowdfunding Unifeel Campaign.
.jpg)
Fig. 1. SEM of CQ microparticles. From left to right: CQ-MPs (with Na stearate), CQ-binary (with Zn gluconate), CQ ternary (with Zn gluconate and lactoferrin).
.jpg)
Fig. 2. Amount of CQ or FPV permeated in 3.5h across excised nasal mucosa (mg cm-2) and concentrations (mM) calculated from the amounts of drug extracted from the mucosa after 3.5h (mean ± SEM).
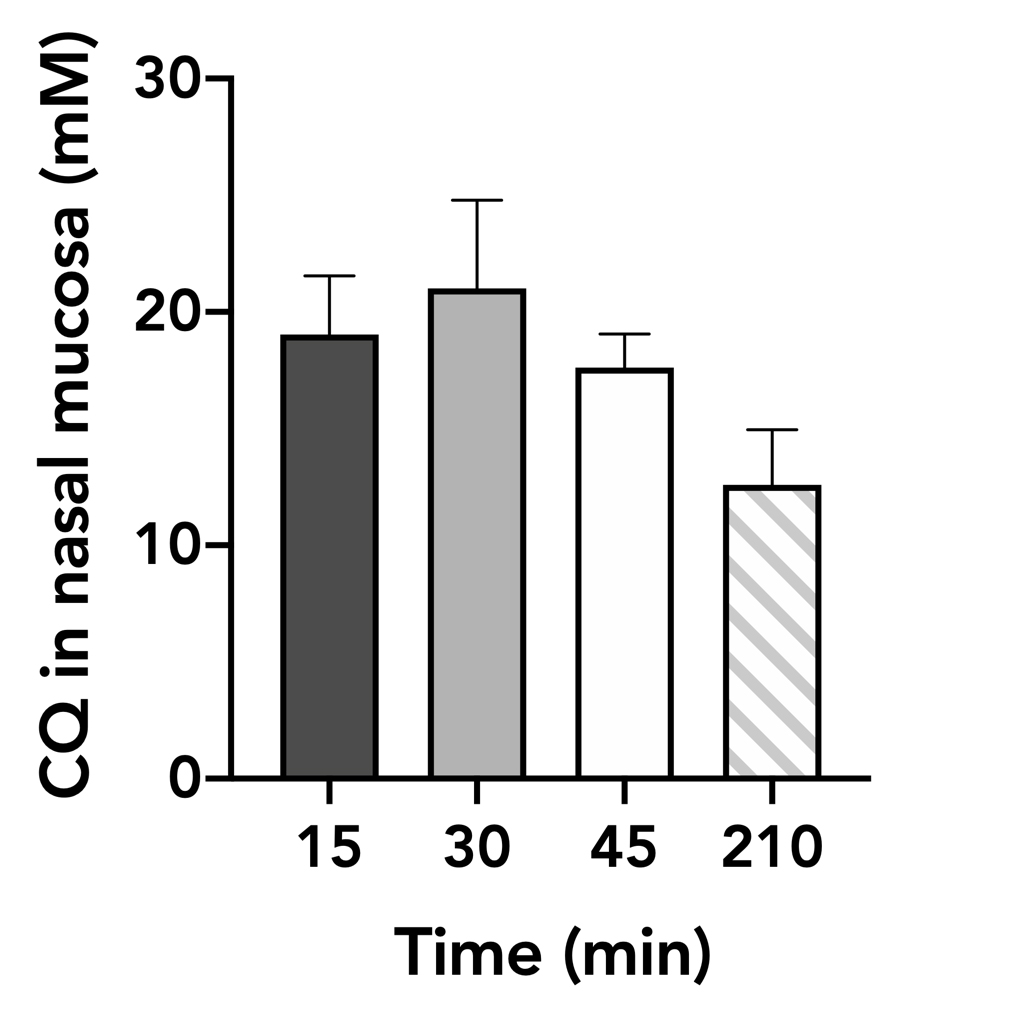
Fig. 3. Chloroquine concentration (mM) in the nasal mucosa as a function of contact time between CQ ternary powder and tissue (mean ± SEM).
Formulation and Delivery - Chemical - Formulation
Category: Poster Abstract
(M1130-12-67) Anti-SARS-CoV-2 Nasal Powders: Manufacturing, Ex Vivo Drug Accumulation/Transport in Rabbit Nasal Mucosa and In Vitro Virus Inhibition
Monday, October 17, 2022
11:30 AM – 12:30 PM ET

Gaia Colombo, PhD
Associate Professor
University of Ferrara
Ferrara, Emilia-Romagna, Italy- SB
Sabrina Banella
University of Ferrara
Ferrara, Emilia-Romagna, Italy
Presenting Author(s)
Main Author(s)
Purpose: Airborne SARS-CoV-2 infection can be tackled by antiviral drug targeted delivery to infected cells of upper airway. Timely antiviral treatment at symptom onset would stop virus spreading to lung and other organs, sparing severe disease. Chloroquine diphosphate (CQ) and favipiravir (FPV) can be repurposed to such objective. Thus, we studied the formulation of CQ and FPV microparticles for in vitro deposition into the upper airway epithelia as aerosol (by nasal powder breath-inspiration in vivo).
Methods: CQ and FPV were independently transformed into microparticles by spray drying from aqueous solutions [1]. 1% (w/w) sodium stearate was added to the composition in both cases (CQ-MPs, FPV-MPs). Additional CQ formulations comprised a zinc salt as drug adjuvant (CQ-binary) and lactoferrin as mucoadhesive agent (CQ-ternary). Powders were characterized for size distribution, morphology, drug content, ex vivo transport across excised rabbit nasal mucosa. The amount of CQ and FPV accumulated in the epithelial cells was measured, also varying the contact time between formulation and mucosa. Powder respirability was preliminarily measured by Fast Screening Impactor, using the RS01® medium resistance dry powder inhaler at 60 L/min air flow rate. Finally, the inhibitory effect of CQ powders against SARS-CoV-2 was determined in vitro on Vero E6 cells. The cells were treated either applying drug after viral inoculum or pre-treating cells with drug before viral inoculum, then treating.
Results: For both APIs, spray drying process formed microparticles with median volume diameter (Dv,0.5) lower than 5 µm, with satisfactory yields (50-85%). For CQ compositions, microparticle morphology was perfectly spherical and surface smooth, when CQ was spray-dried with Na stearate. Zn salt and Zn salt+lactoferrin changed such morphology to corrugated and wrinkled, highlighting a strong effect of the protein on microparticle formation during droplet drying [Fig. 1]. Drug content was according to the theoretical composition for both CQ and FPV, proving drug stability during process. Both APIs crossed quite extensively the rabbit nasal mucosa ex vivo. In detail, the 3.5-h application of an amount of spray-dried powder equivalent to 5 mg of CQ free base (+ 0.1 ml liquid to wet), led to CQ amounts transported per unit area shown in Table I. These amounts corresponded to 40%-63% of CQ initially loaded in the donor. Similarly, almost 60% of loaded FPV (7.5 mg) was found in the receptor compartment at 210 minutes. More interestingly, after extraction from the mucosa and quantification, we found that both APIs highly concentrated inside the mucosal tissue. For CQ, knowing mucosal surface and thickness, drug concentration levels in the tissue were calculated [Fig. 2]. With the ternary powder (CQ + zinc + lactoferrin), we determined that CQ concentrations in the mucosa were higher after shorter contact time between formulation and mucosa (15, 30 and 45 min), as it would happen in vivo [Fig. 3]. Similarly, FPV concentration in the tissue after 30 minutes was 7.4 ± 1.3 mM. With emitted doses >85%, the fine particle fraction (%) of the 3 chloroquine powders ranged from 32.4 ± 2.2% of CQ-binary to 44.4 ± 4.4% of CQ-MPs, likely due to the presence of Na stearate. Although the powder product is for nasal inspiration, a certain degree of respirability is favorable for extending the deposition to the upper airways, including larynx and trachea, where the virus also infects. Finally, when drug treatment in vitro was applied after virus inoculum (MOI 0.05 and 0.005), either once or for 3 consecutive times, the % inhibition of viral replication increased with CQ concentration (from 25 to 75 µM) for all compositions, although not linearly. Compared to one treatment only, three treatments post-infection made the greatest difference in terms of % inhibition, reaching close to 100% inhibition with 3 treatments at 50 µM CQ diphosphate. The powder composition did not substantially affect CQ inhibitory activity. Furthermore, at all CQ concentrations, the 2-hour pre-treatment of cells before virus inoculum, significantly increased the antiviral effect of the subsequent 1 or 3 treatments post-infection. In particular, pre-treatment led to % inhibition values about 3-4 folds or 1.5 folds as higher, respectively when one or three treatments post-infection were carried out.
Conclusion: The investigated spray-dried CQ and FPV microparticles possess the necessary quality attributes to be inspired via the nose and deposited on the upper airway mucosae. Their dissolution on target creates a saturated solution rapidly accumulating the drugs in the infected cells at concentrations of more than 3 orders those inhibiting virus replication in vitro. As nasal doses are much lower than those required if the drug is given systemically, the product’s safety profile is expected high. Thus, the product could be effectively used at first symptoms, even while waiting for the COVID-19 test result.
References: 1. PCT/EP2008/059110; WO 2010/003465 A2
Acknowledgements:This research was funded by part of the generous donations received during the 2021 Crowdfunding Unifeel Campaign.
.jpg)
Fig. 1. SEM of CQ microparticles. From left to right: CQ-MPs (with Na stearate), CQ-binary (with Zn gluconate), CQ ternary (with Zn gluconate and lactoferrin).
.jpg)
Fig. 2. Amount of CQ or FPV permeated in 3.5h across excised nasal mucosa (mg cm-2) and concentrations (mM) calculated from the amounts of drug extracted from the mucosa after 3.5h (mean ± SEM).
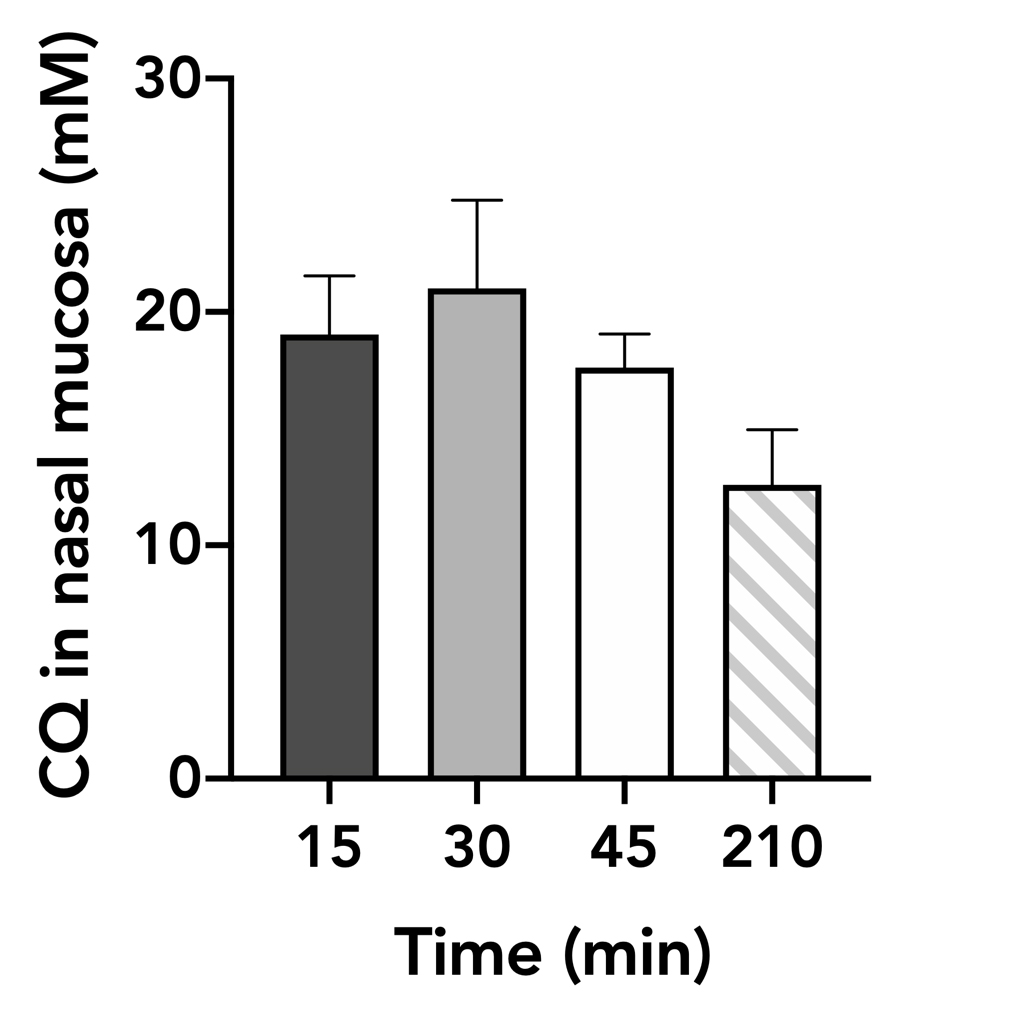
Fig. 3. Chloroquine concentration (mM) in the nasal mucosa as a function of contact time between CQ ternary powder and tissue (mean ± SEM).
