Back

Neurological and Neuropsychiatric Disorders: Other
Traditional Poster Presentation
(159) Neurocognitive Performance in Post-Acute Sequelae of COVID-19 (PASC)
Has Audio
- KL
Kristine Lokken, PhD
Associate Professor and Chief Psychologist
University of Alabama at Birmingham
Birmingham, Alabama, United States
Primary Author(s)
Objective: Describe cognitive function in patients seeking treatment for Post-Acute Sequelae of COVID-19 (PASC).
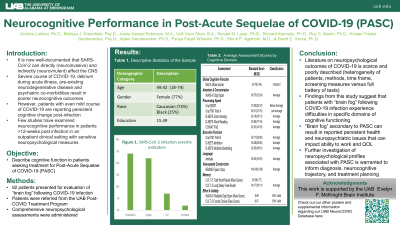
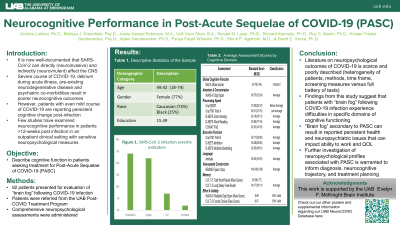
Method: Ninety-two patients underwent neuropsychological evaluation secondary to reported “brain fog” following COVID-19 infection. Patients were referred from the University of Alabama at Birmingham (UAB) Post-COVID Treatment Program. Patients were on average 49 years of age (range: 18-74), female (77%), and White/Caucasian (73%)/Black/AA (25%), with 15.49 years of education (SD = 2.43).
Results: Overall, many patients demonstrated mild impairment on a brief global cognitive screener (MoCA; M = 24.78, SD = 3.46). On specific tasks of cognitive abilities, processing speed was variable; ranging from low average (Oral TMT Part A; M = 88.31, SD = 28.78) to below average (Oral SDMT; M = 72.80, SD = 20.37). Memory for immediate recall was low average (CVLT3-Brief Form (BF) Trials 1-4, M = 88.01, SD = 17.11), while delayed recall was average (CVLT3-BF, M = 94.17, SD = 19.11). Performances on measures of attention/working memory (WAIS-IV Digit Span; M = 96.75, SD = 12.54), executive functioning (Oral TMT Part B; M = 92.71, SD = 28.48), language (COWAT; M = 92.03, SD = 14.19) and visuospatial abilities (RBANS Figure Copy M = 104.04, SD = 16.08) were intact. Performance on embedded validity measures was also intact (RDS [95% valid]; CVLT-3 FC [93% valid]).
Conclusion: Overall, patients with “brain fog” following COVID-19 infection experience difficulties in specific domains of cognitive functioning. Further investigation of neuropsychological profiles associated with PASC is warranted to inform diagnosis, neurocognitive trajectory, and treatment planning.
Method: Ninety-two patients underwent neuropsychological evaluation secondary to reported “brain fog” following COVID-19 infection. Patients were referred from the University of Alabama at Birmingham (UAB) Post-COVID Treatment Program. Patients were on average 49 years of age (range: 18-74), female (77%), and White/Caucasian (73%)/Black/AA (25%), with 15.49 years of education (SD = 2.43).
Results: Overall, many patients demonstrated mild impairment on a brief global cognitive screener (MoCA; M = 24.78, SD = 3.46). On specific tasks of cognitive abilities, processing speed was variable; ranging from low average (Oral TMT Part A; M = 88.31, SD = 28.78) to below average (Oral SDMT; M = 72.80, SD = 20.37). Memory for immediate recall was low average (CVLT3-Brief Form (BF) Trials 1-4, M = 88.01, SD = 17.11), while delayed recall was average (CVLT3-BF, M = 94.17, SD = 19.11). Performances on measures of attention/working memory (WAIS-IV Digit Span; M = 96.75, SD = 12.54), executive functioning (Oral TMT Part B; M = 92.71, SD = 28.48), language (COWAT; M = 92.03, SD = 14.19) and visuospatial abilities (RBANS Figure Copy M = 104.04, SD = 16.08) were intact. Performance on embedded validity measures was also intact (RDS [95% valid]; CVLT-3 FC [93% valid]).
Conclusion: Overall, patients with “brain fog” following COVID-19 infection experience difficulties in specific domains of cognitive functioning. Further investigation of neuropsychological profiles associated with PASC is warranted to inform diagnosis, neurocognitive trajectory, and treatment planning.
