Back
Aging and Dementia: Other
ePoster Presentation
(254) Psychiatric History and Cognitive Impairment in a Subpopulation of Older Adults in a Psychiatric Hospital
- JL
Jacob Lowe, PsyD Clinical Psychology (he/him/his)
Neuropsychology Postdoctoral Fellow
Pine Rest Christian Mental Health Services
Byron Center, Michigan, United States
Primary Author(s)
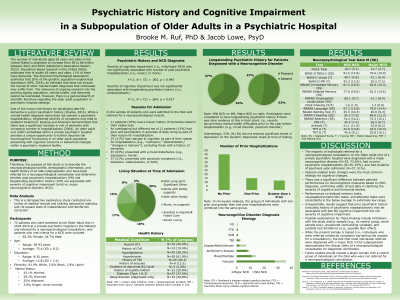
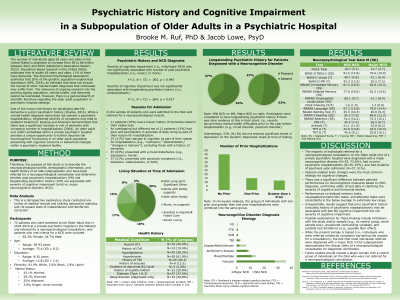
Objective: The purpose of this study is to characterize the neuropsychological (NP) profile of an Older Adult Unit (OAU) subpopulation and determine whether past psychiatric hospitalizations (PH) and longstanding psychiatric history (LPH) are associated with severity of cognitive impairment.
Method: Records were reviewed for a sample of patients admitted to the OAU in a private psychiatric hospital in the Midwest who were referred for a neuropsychological consult in 2018-2019. Only participants diagnosed with a neurocognitive disorder (NCD) were included (74% major, 26% mild). The final sample (N = 72) was 65% female, 82% Caucasian, with a mean age and education level of 75 years (SD =8.23) and 12.8 years (SD = 2.36), respectively. Thirty-seven percent had at least one prior PH. Forty-four percent of the sample had LPH. Participants completed comprehensive NP testing.
Results: A chi-square test of independence with Bonferroni correction was performed to examine the relationships between prior PH and LPH with severity of cognitive impairment (mild versus major NCD). Severity of cognitive impairment was not significantly associated with either prior PH, X2 (1, N = 72) = .005, p = 0.945, or LPH, X2 (1, N = 72) = .604, p = 0.437.
Conclusions: Unexpectedly, neither prior PH nor LPH were associated with severity of cognitive impairment. This suggests that prior psychiatric history may be predictive of presence but not severity of cognitive impairment. Possible explanations for these findings include study/sample limitations, unexplored confounding variables, and possible test limitations. Future studies should include a larger sample with a control group.
Method: Records were reviewed for a sample of patients admitted to the OAU in a private psychiatric hospital in the Midwest who were referred for a neuropsychological consult in 2018-2019. Only participants diagnosed with a neurocognitive disorder (NCD) were included (74% major, 26% mild). The final sample (N = 72) was 65% female, 82% Caucasian, with a mean age and education level of 75 years (SD =8.23) and 12.8 years (SD = 2.36), respectively. Thirty-seven percent had at least one prior PH. Forty-four percent of the sample had LPH. Participants completed comprehensive NP testing.
Results: A chi-square test of independence with Bonferroni correction was performed to examine the relationships between prior PH and LPH with severity of cognitive impairment (mild versus major NCD). Severity of cognitive impairment was not significantly associated with either prior PH, X2 (1, N = 72) = .005, p = 0.945, or LPH, X2 (1, N = 72) = .604, p = 0.437.
Conclusions: Unexpectedly, neither prior PH nor LPH were associated with severity of cognitive impairment. This suggests that prior psychiatric history may be predictive of presence but not severity of cognitive impairment. Possible explanations for these findings include study/sample limitations, unexplored confounding variables, and possible test limitations. Future studies should include a larger sample with a control group.
