Back
Industry Encore Posters
JL1035E: The Economic Impact of Treatment Sequences for Chronic Lymphocytic Leukemia (CLL) in the United States: A Cost of Care and Budget Impact Model of Venetoclax plus Obinutuzumab Sequences for CLL Patients
Saturday, October 22, 2022
10:00 AM – 11:00 AM ET

Michele Puyear, PharmD
Medical Affairs Executive Director
Genentech
Poster Presenter(s)
Background:
Oral targeted regimens (fixed or continuous) have transformed the treatment paradigm in CLL. Venetoclax combined with obinutuzumab (V+O) is the only novel targeted regimen providing a 12-month fixed duration for previously untreated adults with CLL.
Objective:
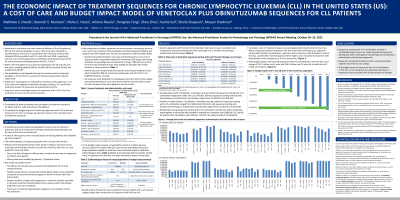
To estimate the total cumulative costs per patient of treatment sequences for adults with CLL (first-line (1L) and retreatment), and to evaluate the budget impact of introducing sequences with V+O in 1L from a United States (US) payer perspective.
Methods:
A partitioned survival model was developed to assess costs of treatment sequences with up to three lines of therapy. A total of 249 sequences were included based on NCCN guidelines and validation by clinical experts. The model adopted a US payer perspective with a 10-year time horizon. Patients were distributed into five states (i.e. 1L, 2L, 3L, supportive care and death) based on efficacy data from clinical trials and real-world data. Cost components included: treatment and administration, monitoring, terminal care, tumor lysis syndrome prophylaxis (venetoclax-based therapies) and adverse events. Model outputs included 10-year cumulative costs per patient and 5-year budget impact after market entry of sequences with 1L V+O.
Results:
Overall, sequences with 1L V+O had lower 10-year cumulative costs compared to sequences starting with other novel agents (i.e. ibrutinib, acalabrutinib). Among patients with 17p deletion, cumulative costs per patient of sequences starting with V+O ranged from $935,781 to $1,345,96; whereas sequences starting with ibrutinib or acalabrutinib ranged from $1,426,924 to $1,906,544. Similarly, in adults without 17p deletion, cumulative costs per patient of sequences starting with V+O ranged from $690,346 to $951,633; and sequences starting with ibrutinib or acalabrutinib ranged from $1,720,745 to $1,976,767. Additionally, retreatment with a venetoclax-based regimen in 2L or 3L often resulted in sequences with the lowest cost. Total budget impact of introducing sequences with V+O in 1L led to cost savings of $12.5 million over 5 years for a health plan of 1 million US members.
Conclusions:
In our model, sequences starting with V+O resulted in considerably lower costs compared to sequences starting with novel agents administered until disease progression. Sequences including retreatment with a venetoclax-based regimen also led to cost savings. The budget impact of sequences with V+O in 1L is expected to be cost saving due to substantial reductions in treatment costs associated with a finite duration therapy.
Oral targeted regimens (fixed or continuous) have transformed the treatment paradigm in CLL. Venetoclax combined with obinutuzumab (V+O) is the only novel targeted regimen providing a 12-month fixed duration for previously untreated adults with CLL.
Objective:
To estimate the total cumulative costs per patient of treatment sequences for adults with CLL (first-line (1L) and retreatment), and to evaluate the budget impact of introducing sequences with V+O in 1L from a United States (US) payer perspective.
Methods:
A partitioned survival model was developed to assess costs of treatment sequences with up to three lines of therapy. A total of 249 sequences were included based on NCCN guidelines and validation by clinical experts. The model adopted a US payer perspective with a 10-year time horizon. Patients were distributed into five states (i.e. 1L, 2L, 3L, supportive care and death) based on efficacy data from clinical trials and real-world data. Cost components included: treatment and administration, monitoring, terminal care, tumor lysis syndrome prophylaxis (venetoclax-based therapies) and adverse events. Model outputs included 10-year cumulative costs per patient and 5-year budget impact after market entry of sequences with 1L V+O.
Results:
Overall, sequences with 1L V+O had lower 10-year cumulative costs compared to sequences starting with other novel agents (i.e. ibrutinib, acalabrutinib). Among patients with 17p deletion, cumulative costs per patient of sequences starting with V+O ranged from $935,781 to $1,345,96; whereas sequences starting with ibrutinib or acalabrutinib ranged from $1,426,924 to $1,906,544. Similarly, in adults without 17p deletion, cumulative costs per patient of sequences starting with V+O ranged from $690,346 to $951,633; and sequences starting with ibrutinib or acalabrutinib ranged from $1,720,745 to $1,976,767. Additionally, retreatment with a venetoclax-based regimen in 2L or 3L often resulted in sequences with the lowest cost. Total budget impact of introducing sequences with V+O in 1L led to cost savings of $12.5 million over 5 years for a health plan of 1 million US members.
Conclusions:
In our model, sequences starting with V+O resulted in considerably lower costs compared to sequences starting with novel agents administered until disease progression. Sequences including retreatment with a venetoclax-based regimen also led to cost savings. The budget impact of sequences with V+O in 1L is expected to be cost saving due to substantial reductions in treatment costs associated with a finite duration therapy.

