Back
Industry Encore Posters
JL1036E: The Efficacy of Enzalutamide (ENZA) Plus Androgen Deprivation Therapy (ADT) on Oligometastatic Hormone-Sensitive Prostate Cancer: Extended Post Hoc Analysis of ARCHES
Saturday, October 22, 2022
10:00 AM – 11:00 AM ET
- CW
Charlene G. Whittlesey, PharmD, BCPS
Senior Medical Science Liaison
Astellas Pharma
Tampa, Florida, United States
Poster Presenter(s)
Background:
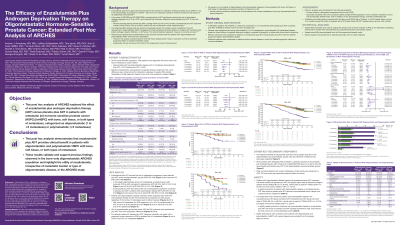
In ARCHES (NCT02677896), ENZA + ADT reduced the risk of radiographic progression and improved secondary clinical outcomes in patients with metastatic hormone-sensitive prostate cancer (mHSPC) over placebo (PBO) + ADT. A previous post hoc analysis demonstrated the efficacy of ENZA + ADT on bone-only oligometastatic disease but excluded soft tissue disease to control for the influence of variable metastatic spread. However, soft tissue metastases are often present in oligometastatic HSPC patients with or without bone metastases. Therefore, it is important to assess their influence on the disease and clinical outcomes. This extended post hoc analysis evaluated the efficacy of ENZA + ADT in patients with oligometastatic HSPC compared to polymetastatic HSPC in the ARCHES overall intent-to-treat (ITT) population, which included those with bone, soft tissue or both types of metastases.
Methods:
Patients with mHSPC (n=1150) were randomized 1:1 to ENZA (160 mg/day) + ADT or PBO + ADT, stratified by disease volume and prior docetaxel chemotherapy. Eligible patients in this post hoc analysis were those with bone (n=512), soft tissue (n=96), or both types of metastases (n=458), categorized as oligometastatic (1–≤5 metastases) or as polymetastatic (≥6 metastases) based on central review at screening. Efficacy outcomes were compared across treatment arms. Additional analyses were conducted on patients without visceral disease to control for possible prognostic influence of visceral metastases (n=927).
Results:
Of the ARCHES ITT population with soft tissue, bone, or both types of metastases (n=1,066), the largest oligometastatic subgroup was patients with ≤5 metastases (ENZA + ADT, n=270; PBO + ADT, n=250). Baseline characteristics were generally comparable between treatment arms and across subgroups. When compared to PBO + ADT, ENZA + ADT improved rPFS and secondary endpoints in oligometastatic patients with ≤5 metastases in the ITT population (Table). Similar results were observed across other patient oligometastatic subgroups (1–≤4 metastases) as well as in patients with polymetastatic disease (≥6 metastases). The safety profile of ENZA + ADT versus PBO + ADT was similar across subgroups and consistent with previous findings. In addition, the efficacy and safety profile observed in the ITT population oligometastatic and polymetastatic subgroups was maintained in patients without visceral metastases.
Conclusion:
This post hoc analysis demonstrates that ENZA + ADT provided clinical benefit to patients with oligometastatic and polymetastatic HSPC, with bone, soft tissue, or both types of metastases. Overall, these results validate and support previous findings observed in the bone-only oligometastatic ARCHES population and highlight the utility of enzalutamide irrespective of metastatic burden or type of oligometastatic disease in the ARCHES study.
Table
JL1036E Table
To view the table, please click on this link from the e-poster gallery on jadprolive.com
Funding: Funding for this research was provided by Pfizer, Inc. and Astellas Pharma, Inc.
Acknowledgements: Medical writing and editorial support funded by both sponsor companies was provided by Folabomi Oladosu, PhD, and Jane Beck, MA, from Complete HealthVizion, and Adam Anazim, BSc, from Onyx, a Prime Global agency.
In ARCHES (NCT02677896), ENZA + ADT reduced the risk of radiographic progression and improved secondary clinical outcomes in patients with metastatic hormone-sensitive prostate cancer (mHSPC) over placebo (PBO) + ADT. A previous post hoc analysis demonstrated the efficacy of ENZA + ADT on bone-only oligometastatic disease but excluded soft tissue disease to control for the influence of variable metastatic spread. However, soft tissue metastases are often present in oligometastatic HSPC patients with or without bone metastases. Therefore, it is important to assess their influence on the disease and clinical outcomes. This extended post hoc analysis evaluated the efficacy of ENZA + ADT in patients with oligometastatic HSPC compared to polymetastatic HSPC in the ARCHES overall intent-to-treat (ITT) population, which included those with bone, soft tissue or both types of metastases.
Methods:
Patients with mHSPC (n=1150) were randomized 1:1 to ENZA (160 mg/day) + ADT or PBO + ADT, stratified by disease volume and prior docetaxel chemotherapy. Eligible patients in this post hoc analysis were those with bone (n=512), soft tissue (n=96), or both types of metastases (n=458), categorized as oligometastatic (1–≤5 metastases) or as polymetastatic (≥6 metastases) based on central review at screening. Efficacy outcomes were compared across treatment arms. Additional analyses were conducted on patients without visceral disease to control for possible prognostic influence of visceral metastases (n=927).
Results:
Of the ARCHES ITT population with soft tissue, bone, or both types of metastases (n=1,066), the largest oligometastatic subgroup was patients with ≤5 metastases (ENZA + ADT, n=270; PBO + ADT, n=250). Baseline characteristics were generally comparable between treatment arms and across subgroups. When compared to PBO + ADT, ENZA + ADT improved rPFS and secondary endpoints in oligometastatic patients with ≤5 metastases in the ITT population (Table). Similar results were observed across other patient oligometastatic subgroups (1–≤4 metastases) as well as in patients with polymetastatic disease (≥6 metastases). The safety profile of ENZA + ADT versus PBO + ADT was similar across subgroups and consistent with previous findings. In addition, the efficacy and safety profile observed in the ITT population oligometastatic and polymetastatic subgroups was maintained in patients without visceral metastases.
Conclusion:
This post hoc analysis demonstrates that ENZA + ADT provided clinical benefit to patients with oligometastatic and polymetastatic HSPC, with bone, soft tissue, or both types of metastases. Overall, these results validate and support previous findings observed in the bone-only oligometastatic ARCHES population and highlight the utility of enzalutamide irrespective of metastatic burden or type of oligometastatic disease in the ARCHES study.
Table
JL1036E Table
To view the table, please click on this link from the e-poster gallery on jadprolive.com
Funding: Funding for this research was provided by Pfizer, Inc. and Astellas Pharma, Inc.
Acknowledgements: Medical writing and editorial support funded by both sponsor companies was provided by Folabomi Oladosu, PhD, and Jane Beck, MA, from Complete HealthVizion, and Adam Anazim, BSc, from Onyx, a Prime Global agency.

