Back

Industry Encore Posters
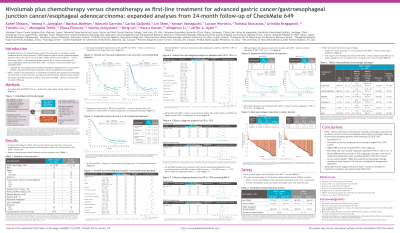
JL1020E: Nivolumab plus chemotherapy versus chemotherapy as first-line treatment for advanced gastric cancer/gastroesophageal junction cancer/esophageal adenocarcinoma: expanded analyses from 24-month follow-up of CheckMate 649
Saturday, October 22, 2022
10:00 AM – 11:00 AM ET
Has Audio

Rajni Kannan, BS, MS, RN, ANP-C (she/her/hers)
Associate Director, Medical Scientist
Bristol Myers Squibb, New Jersey, United States
Poster Presenter(s)
Background:
CheckMate 649 is a randomized, global phase 3 study of first-line (1L) programmed death-1 (PD-1) inhibitor–based therapies in advanced non-HER2-positive gastric cancer/gastroesophageal junction cancer/esophageal adenocarcinoma (GC/GEJC/EAC) that demonstrated superior overall survival (OS) with nivolumab (NIVO) + chemotherapy (chemo) vs chemo, leading to approvals in the US and other countries. Clinically meaningful long-term survival benefit with NIVO + chemo vs chemo was observed with 24 months (mo) of minimum follow-up in all randomized patients (pts) for both OS (HR 0.79 [95% CI 0.71–0.88]) and progression-free survival (PFS; HR 0.79 [95% CI 0.70–0.89]; Janjigian YY et al; ESMO 2021). We present expanded analyses of NIVO + chemo vs chemo with minimum follow-up of 24 mo.
Methods:
Adults with previously untreated, unresectable advanced or metastatic GC/GEJC/EAC were enrolled regardless of PD-ligand (L)1 expression. Pts with known HER2-positive status were excluded. Pts were randomized to NIVO (360 mg Q3W or 240 mg Q2W) + chemo (XELOX Q3W or FOLFOX Q2W), NIVO 1 mg/kg + IPI 3 mg/kg Q3W (4 doses, then NIVO 240 mg Q2W), or chemo. Dual primary endpoints were OS and PFS (per blinded independent central review) in pts with PD-L1 combined positive score (CPS) ≥ 5 for NIVO + chemo vs chemo. Hierarchically tested secondary endpoints included OS in NIVO + chemo vs chemo (PD-L1 CPS ≥ 1, then all randomized).
Results:
Of 2031 pts, 1581 were randomized to NIVO + chemo or chemo. In all randomized pts, 41% of pts (NIVO + chemo) and 44% of pts (chemo) received subsequent therapy. Median PFS2 (time from randomization to progression after subsequent systemic therapy, initiation of second subsequent systemic therapy, or death, whichever is earlier) was 12.2 (95% CI 11.3–13.5) mo with NIVO + chemo and 10.4 (95% CI 9.7–11.2) mo with chemo (HR 0.75 [95% CI 0.67–0.84]). 51% of pts (NIVO + chemo) and 43% of pts (chemo) had > 50% reduction from baseline in tumor burden, while 24% and 17% had > 80% reduction, respectively. The HR (95% CI) for OS was 0.66 (0.56–0.77) among pts with a PD-L1 CPS ≥ 10 (median OS for NIVO + chemo vs chemo: 15.0 [95% CI 13.7–16.7] vs 10.9 [95% CI 9.8–11.9] mo). OS benefit was observed with NIVO + chemo vs chemo across multiple additional subgroups, and these data will be presented. No new safety signals were identified. The majority of the treatment-related adverse events with potential immunologic etiology were grade 1 or 2 and grade 3 or 4 events were reported in ≤ 5% of pts in both treatment arms.
Conclusions:
NIVO + chemo continued to demonstrate clinically meaningful efficacy and an acceptable safety profile with longer follow-up, further supporting the use of NIVO + chemo as a standard 1L therapy in previously untreated pts with advanced GC/GEJC/EAC.
© 2022 American Society of Clinical Oncology, Inc. Reused with permission. This abstract was accepted and previously presented at the 2022 Gastrointestinal Cancers Symposium. All rights reserved.
CheckMate 649 is a randomized, global phase 3 study of first-line (1L) programmed death-1 (PD-1) inhibitor–based therapies in advanced non-HER2-positive gastric cancer/gastroesophageal junction cancer/esophageal adenocarcinoma (GC/GEJC/EAC) that demonstrated superior overall survival (OS) with nivolumab (NIVO) + chemotherapy (chemo) vs chemo, leading to approvals in the US and other countries. Clinically meaningful long-term survival benefit with NIVO + chemo vs chemo was observed with 24 months (mo) of minimum follow-up in all randomized patients (pts) for both OS (HR 0.79 [95% CI 0.71–0.88]) and progression-free survival (PFS; HR 0.79 [95% CI 0.70–0.89]; Janjigian YY et al; ESMO 2021). We present expanded analyses of NIVO + chemo vs chemo with minimum follow-up of 24 mo.
Methods:
Adults with previously untreated, unresectable advanced or metastatic GC/GEJC/EAC were enrolled regardless of PD-ligand (L)1 expression. Pts with known HER2-positive status were excluded. Pts were randomized to NIVO (360 mg Q3W or 240 mg Q2W) + chemo (XELOX Q3W or FOLFOX Q2W), NIVO 1 mg/kg + IPI 3 mg/kg Q3W (4 doses, then NIVO 240 mg Q2W), or chemo. Dual primary endpoints were OS and PFS (per blinded independent central review) in pts with PD-L1 combined positive score (CPS) ≥ 5 for NIVO + chemo vs chemo. Hierarchically tested secondary endpoints included OS in NIVO + chemo vs chemo (PD-L1 CPS ≥ 1, then all randomized).
Results:
Of 2031 pts, 1581 were randomized to NIVO + chemo or chemo. In all randomized pts, 41% of pts (NIVO + chemo) and 44% of pts (chemo) received subsequent therapy. Median PFS2 (time from randomization to progression after subsequent systemic therapy, initiation of second subsequent systemic therapy, or death, whichever is earlier) was 12.2 (95% CI 11.3–13.5) mo with NIVO + chemo and 10.4 (95% CI 9.7–11.2) mo with chemo (HR 0.75 [95% CI 0.67–0.84]). 51% of pts (NIVO + chemo) and 43% of pts (chemo) had > 50% reduction from baseline in tumor burden, while 24% and 17% had > 80% reduction, respectively. The HR (95% CI) for OS was 0.66 (0.56–0.77) among pts with a PD-L1 CPS ≥ 10 (median OS for NIVO + chemo vs chemo: 15.0 [95% CI 13.7–16.7] vs 10.9 [95% CI 9.8–11.9] mo). OS benefit was observed with NIVO + chemo vs chemo across multiple additional subgroups, and these data will be presented. No new safety signals were identified. The majority of the treatment-related adverse events with potential immunologic etiology were grade 1 or 2 and grade 3 or 4 events were reported in ≤ 5% of pts in both treatment arms.
Conclusions:
NIVO + chemo continued to demonstrate clinically meaningful efficacy and an acceptable safety profile with longer follow-up, further supporting the use of NIVO + chemo as a standard 1L therapy in previously untreated pts with advanced GC/GEJC/EAC.
© 2022 American Society of Clinical Oncology, Inc. Reused with permission. This abstract was accepted and previously presented at the 2022 Gastrointestinal Cancers Symposium. All rights reserved.

