Back
Industry Encore Posters
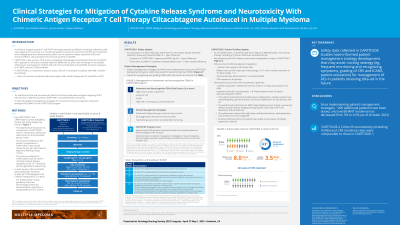
JL1005E: Clinical Strategies for Mitigation of Cytokine Release Syndrome and Neurotoxicity With Chimeric Antigen Receptor T Cell Therapy Ciltacabtagene Autoleucel in Multiple Myeloma
Saturday, October 22, 2022
10:00 AM – 11:00 AM ET

Patrick Stoy, PhD, BS
Senior Medical Science Liaison
Janssen Biotech, Inc
Poster Presenter(s)
As chimeric antigen receptor T cell (CAR-T) therapies expand to different indications with new targets and constructs, it is crucial that patients receive the maximum benefit from treatment while mitigating serious adverse events (AEs) such as cytokine release syndrome (CRS) and immune effector cell–associated neurotoxicity syndrome (ICANS). The aims of this analysis are to characterize CRS and neurotoxicity data for the B-cell maturation antigen–targeting CAR-T ciltacabtagene autoleucel (cilta-cel) from two multiple myeloma (MM) clinical trials, CARTITUDE-1 and CARTITUDE-2 cohort B, as well as to describe patient management strategies for movement and neurocognitive treatment-emergent AEs (MNTs) in the CARTITUDE program.
CARTITUDE-1 is a phase 1b/2 study in patients with relapsed or refractory MM (RRMM) with ≥3 prior lines of therapy or are double refractory to a proteasome inhibitor (PI) and immunomodulatory drug (IMID), and prior exposure to PI, IMID, and anti-CD38 antibody. As of July 2021 (~2-year median follow-up), no new safety signals were observed relative to previously reported data, including no MNTs since an ~1-year median follow-up. After implementation of patient management strategies (Figure) for MNT across the development program (including early aggressive treatment of CRS and ICANS, and extended monitoring and reporting of neurotoxicity) informed by analysis of 2 or more risk factors (eg, high baseline tumor burden, previous ICANS, grade ≥2 CRS, and/or high CAR-T cell expansion and persistence), approximately 200 patients have been dosed with cilta-cel across the CARTITUDE clinical development program as of October 2021 and overall MNT incidence has decreased to 0.5%.
In CARTITUDE-2 cohort B, 19 patients with MM after early relapse following one line of prior therapy including a PI and an IMID have received cilta-cel as of October 2021. Neurotoxicity (26%) and CRS (84%) incidence rates were comparable to those in CARTITUDE-1. One patient experienced grade 3 MNT; this patient was treated with high-dose methylprednisolone, plasmapheresis, and intravenous immunoglobin and was reported to be stable with some improvements at data cutoff.
Data collected in CARTITUDE studies have informed patient management strategy development that may assist nursing strategy (eg, frequent monitoring and recognizing symptoms, grading of CRS and ICANS, patient education) for management of AEs in patients receiving cilta-cel in the future.
CARTITUDE-1 is a phase 1b/2 study in patients with relapsed or refractory MM (RRMM) with ≥3 prior lines of therapy or are double refractory to a proteasome inhibitor (PI) and immunomodulatory drug (IMID), and prior exposure to PI, IMID, and anti-CD38 antibody. As of July 2021 (~2-year median follow-up), no new safety signals were observed relative to previously reported data, including no MNTs since an ~1-year median follow-up. After implementation of patient management strategies (Figure) for MNT across the development program (including early aggressive treatment of CRS and ICANS, and extended monitoring and reporting of neurotoxicity) informed by analysis of 2 or more risk factors (eg, high baseline tumor burden, previous ICANS, grade ≥2 CRS, and/or high CAR-T cell expansion and persistence), approximately 200 patients have been dosed with cilta-cel across the CARTITUDE clinical development program as of October 2021 and overall MNT incidence has decreased to 0.5%.
In CARTITUDE-2 cohort B, 19 patients with MM after early relapse following one line of prior therapy including a PI and an IMID have received cilta-cel as of October 2021. Neurotoxicity (26%) and CRS (84%) incidence rates were comparable to those in CARTITUDE-1. One patient experienced grade 3 MNT; this patient was treated with high-dose methylprednisolone, plasmapheresis, and intravenous immunoglobin and was reported to be stable with some improvements at data cutoff.
Data collected in CARTITUDE studies have informed patient management strategy development that may assist nursing strategy (eg, frequent monitoring and recognizing symptoms, grading of CRS and ICANS, patient education) for management of AEs in patients receiving cilta-cel in the future.

