Back
APSHO Patient Perspective Posters
JL1008P: Experts by Experience: Paving a Pathway to Engage Underrepresented Oncology Patients in the Research Ecosystem
Saturday, October 22, 2022
10:00 AM – 11:00 AM ET

Kathleen D. Gallagher, MPH (she/her/hers)
Vice President Health Service Research
Patient Advocate Foundation
Hampton, Virginia, United States
Poster Presenter(s)
Background:
Limited engagement of under-resourced and historically underrepresented populations in research exacerbates existing disparities in health outcomes and deepens mistrust of systems, research, and researchers. While oncology patients are often asked to participate in disparity-focused research, there is little evidence supporting their equitable inclusion in the research development process. As a result, research prioritization and methodology lack this group’s unique perspective and dissemination efforts never reach this population or fail in their translation—preventing participants from understanding the importance and/or relevance of the results. Gaps in research engagement are due to logistical, literacy, access, motivation, and trust challenges compounded by the fact that patients often do not understand the research itself and why their involvement in this process is important and necessary to achieve tangible results.
Process:
To bridge this gap, in May 2021 we surveyed via email a diverse network of 27,541 patients served by Patient Advocate Foundation with a history of access and affordability challenges. Our purpose was to capture baseline data about patients’ experiences, attitudes, skills and barriers to participating in the research ecosystem. Eleven percent of those invited to participate completed the survey (n = 2,911); 32% of the respondents (n = 940) identified as cancer patients.
Findings:
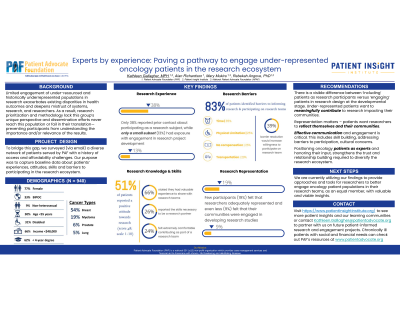
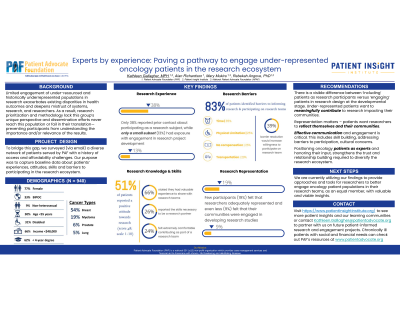
Survey respondents were female (77%); non-heterosexual (9%); non-White (33%); aged <55 years (30%); <4-year degree (62%); annual income <$48,000 (66%); retired (37%) or disabled (31%). The most common cancer types reported were breast (54%), myeloma (19%), prostate (6%) and lung (5%).
Thirty-eight percent were previously contacted about participating as a subject in a research project; 13% reported prior engagement in research development. Respondent attitude towards research (score >8, range 1-10) was positive (51%); 66% felt they had valuable experience to share with researchers and 26% reported having the skills to be a patient research partner. One quarter (24%) felt ‘extremely comfortable’ contributing as part of a research team and 87% stated they would join a research team if technology training were provided. Eighty-three percent identified barriers to informing research: time (35%), disability/physical limitation (25%), no compensation (25%) and transportation (20%) were top concerns. Resolution of barriers would increase participation willingness (39%). Few participants felt that researchers adequately represented (19%) or engaged their communities (9%) in research studies.
Recommendations:
There is a visible difference between ‘including’ patients as research participants versus ‘engaging’ patients in research design. Under-represented patients want to meaningfully contribute to research impacting their communities. They generally feel they have the skills required and are enthusiastic about the opportunity, especially if their specific concerns or barriers are proactively addressed. Given this, researchers need to find ways to reach, effectively communicate, and meaningfully engage diverse patient populations at the development stage. These efforts should circumvent tokenism, foster transparency, and address individual barriers to participation. Positioning oncology patients as experts and honoring their input, strengthens the trust and relationship building required to diversity research—specifically clinical trials. We are currently utilizing our findings to provide approaches and tools for researchers to better engage oncology patient populations in their research teams, as an equal member, with valuable and viable insights.
Limited engagement of under-resourced and historically underrepresented populations in research exacerbates existing disparities in health outcomes and deepens mistrust of systems, research, and researchers. While oncology patients are often asked to participate in disparity-focused research, there is little evidence supporting their equitable inclusion in the research development process. As a result, research prioritization and methodology lack this group’s unique perspective and dissemination efforts never reach this population or fail in their translation—preventing participants from understanding the importance and/or relevance of the results. Gaps in research engagement are due to logistical, literacy, access, motivation, and trust challenges compounded by the fact that patients often do not understand the research itself and why their involvement in this process is important and necessary to achieve tangible results.
Process:
To bridge this gap, in May 2021 we surveyed via email a diverse network of 27,541 patients served by Patient Advocate Foundation with a history of access and affordability challenges. Our purpose was to capture baseline data about patients’ experiences, attitudes, skills and barriers to participating in the research ecosystem. Eleven percent of those invited to participate completed the survey (n = 2,911); 32% of the respondents (n = 940) identified as cancer patients.
Findings:
Survey respondents were female (77%); non-heterosexual (9%); non-White (33%); aged <55 years (30%); <4-year degree (62%); annual income <$48,000 (66%); retired (37%) or disabled (31%). The most common cancer types reported were breast (54%), myeloma (19%), prostate (6%) and lung (5%).
Thirty-eight percent were previously contacted about participating as a subject in a research project; 13% reported prior engagement in research development. Respondent attitude towards research (score >8, range 1-10) was positive (51%); 66% felt they had valuable experience to share with researchers and 26% reported having the skills to be a patient research partner. One quarter (24%) felt ‘extremely comfortable’ contributing as part of a research team and 87% stated they would join a research team if technology training were provided. Eighty-three percent identified barriers to informing research: time (35%), disability/physical limitation (25%), no compensation (25%) and transportation (20%) were top concerns. Resolution of barriers would increase participation willingness (39%). Few participants felt that researchers adequately represented (19%) or engaged their communities (9%) in research studies.
Recommendations:
There is a visible difference between ‘including’ patients as research participants versus ‘engaging’ patients in research design. Under-represented patients want to meaningfully contribute to research impacting their communities. They generally feel they have the skills required and are enthusiastic about the opportunity, especially if their specific concerns or barriers are proactively addressed. Given this, researchers need to find ways to reach, effectively communicate, and meaningfully engage diverse patient populations at the development stage. These efforts should circumvent tokenism, foster transparency, and address individual barriers to participation. Positioning oncology patients as experts and honoring their input, strengthens the trust and relationship building required to diversity research—specifically clinical trials. We are currently utilizing our findings to provide approaches and tools for researchers to better engage oncology patient populations in their research teams, as an equal member, with valuable and viable insights.

