Back

Industry Encore Posters
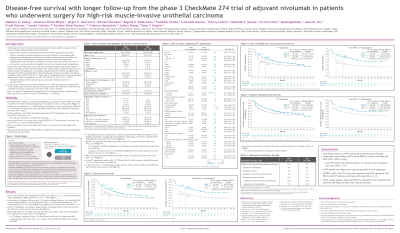
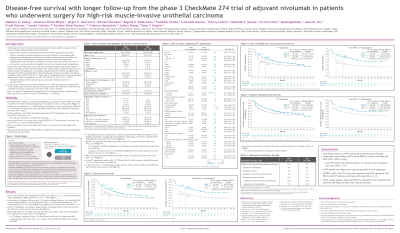
JL1007E: Disease-free survival with longer follow-up from the phase 3 CheckMate 274 trial of adjuvant nivolumab in patients who underwent surgery for high-risk muscle-invasive urothelial carcinoma
Saturday, October 22, 2022
10:00 AM – 11:00 AM ET
Has Audio

Nancy Gudex, MSN, ANP-BC, AOCNP® (she/her/hers)
Senior Medical Science Liaison
Bristol Myers Squibb
Malone, Wisconsin, United States
Poster Presenter(s)
Background:
The standard of care for muscle-invasive urothelial carcinoma (MIUC) is surgery ± cisplatin-based neoadjuvant chemotherapy (NAC), although >50% of patients experience metastatic recurrence. There is an unmet need in this population as no evidence supports adjuvant chemotherapy in patients after NAC and the level of evidence is low for patients who have not received NAC (except for urothelial carcinoma of the renal pelvis and ureter). Furthermore, some patients are ineligible or decline cisplatin-based chemotherapy. In the CheckMate 274 trial of adjuvant nivolumab versus placebo in patients with MIUC at high risk of recurrence after radical surgery (minimum follow-up in the intention-to-treat [ITT] population: 5.9 months), disease-free survival (DFS) was significantly improved with nivolumab versus placebo both in the ITT population (HR, 0.70; 98.22% CI, 0.55-0.90; P< 0.001) and in the population with tumor PD-L1 expression ≥1% (HR, 0.55; 98.72% CI, 0.35-0.85; P< 0.001). We report DFS outcomes with longer follow-up.
Methods:
CheckMate 274 is a phase 3, randomized, double-blind, multicenter trial of nivolumab (anti-PD-1 antibody) versus placebo in high-risk MIUC (bladder, ureter, renal pelvis) after radical surgery. Patients were randomized 1:1 to nivolumab 240 mg intravenously Q2W or placebo for ≤1 year of adjuvant treatment, and stratified by nodal status, prior neoadjuvant cisplatin, and PD-L1 status. Patients had radical surgery within 120 days ± neoadjuvant cisplatin or were ineligible/declined cisplatin-based chemotherapy, had evidence of urothelial carcinoma at high risk of recurrence per pathologic staging, were disease-free by imaging, and had Eastern Cooperative Oncology Group performance status (ECOG PS) ≤1. Primary endpoints were DFS in all randomized patients (ITT population) and in patients with PD-L1 ≥1%. DFS was also evaluated in prespecified subgroups. Non–urothelial tract recurrence-free survival (NUTRFS) in ITT patients and in patients with PD-L1 ≥1% was a secondary endpoint. Distant metastasis-free survival (DMFS) was an exploratory endpoint.
Results:
Overall, 353 patients were randomized to nivolumab (PD-L1 ≥1%, n=140) and 356 to placebo (PD-L1 ≥1%, n=142). With 5 months additional follow-up, DFS benefit with nivolumab versus placebo was maintained in ITT patients (minimum follow-up, 11.0 months; median follow-up, 24.4 months [nivolumab] and 22.5 months [placebo]) and patients with PD-L1 ≥1% (minimum follow-up, 11.4 months; median follow-up, 25.5 months [nivolumab] and 22.4 months [placebo]; Table). DFS probability at 12 months was 63.5% with nivolumab and 46.9% with placebo in ITT patients. Among patients with PD-L1 ≥1%, DFS probability at 12 months was 67.6% with nivolumab and 46.3% with placebo. Improvement in DFS was observed with nivolumab versus placebo for most subgroups analyzed, including age, sex, ECOG PS, nodal status, use of prior cisplatin-based chemotherapy, and PD-L1 status. NUTRFS and DMFS were also improved with nivolumab versus placebo in both ITT patients and those with PD-L1 ≥1% (Table).
Conclusions:
With longer follow-up, nivolumab continued to demonstrate clinically meaningful improvement in DFS versus placebo for patients with high-risk MIUC after radical surgery, both in ITT patients and in patients with PD-L1 ≥1%. DFS benefit was observed in most prespecified subgroups. NUTRFS and DMFS were also improved with nivolumab compared with placebo in both ITT patients and those with PD-L1 ≥1%. These results support adjuvant nivolumab as a standard-of-care treatment for patients with high-risk MIUC after radical surgery.
Table
JL1007E Table
To view the table, please click on this link from the e-poster gallery on jadprolive.com
The standard of care for muscle-invasive urothelial carcinoma (MIUC) is surgery ± cisplatin-based neoadjuvant chemotherapy (NAC), although >50% of patients experience metastatic recurrence. There is an unmet need in this population as no evidence supports adjuvant chemotherapy in patients after NAC and the level of evidence is low for patients who have not received NAC (except for urothelial carcinoma of the renal pelvis and ureter). Furthermore, some patients are ineligible or decline cisplatin-based chemotherapy. In the CheckMate 274 trial of adjuvant nivolumab versus placebo in patients with MIUC at high risk of recurrence after radical surgery (minimum follow-up in the intention-to-treat [ITT] population: 5.9 months), disease-free survival (DFS) was significantly improved with nivolumab versus placebo both in the ITT population (HR, 0.70; 98.22% CI, 0.55-0.90; P< 0.001) and in the population with tumor PD-L1 expression ≥1% (HR, 0.55; 98.72% CI, 0.35-0.85; P< 0.001). We report DFS outcomes with longer follow-up.
Methods:
CheckMate 274 is a phase 3, randomized, double-blind, multicenter trial of nivolumab (anti-PD-1 antibody) versus placebo in high-risk MIUC (bladder, ureter, renal pelvis) after radical surgery. Patients were randomized 1:1 to nivolumab 240 mg intravenously Q2W or placebo for ≤1 year of adjuvant treatment, and stratified by nodal status, prior neoadjuvant cisplatin, and PD-L1 status. Patients had radical surgery within 120 days ± neoadjuvant cisplatin or were ineligible/declined cisplatin-based chemotherapy, had evidence of urothelial carcinoma at high risk of recurrence per pathologic staging, were disease-free by imaging, and had Eastern Cooperative Oncology Group performance status (ECOG PS) ≤1. Primary endpoints were DFS in all randomized patients (ITT population) and in patients with PD-L1 ≥1%. DFS was also evaluated in prespecified subgroups. Non–urothelial tract recurrence-free survival (NUTRFS) in ITT patients and in patients with PD-L1 ≥1% was a secondary endpoint. Distant metastasis-free survival (DMFS) was an exploratory endpoint.
Results:
Overall, 353 patients were randomized to nivolumab (PD-L1 ≥1%, n=140) and 356 to placebo (PD-L1 ≥1%, n=142). With 5 months additional follow-up, DFS benefit with nivolumab versus placebo was maintained in ITT patients (minimum follow-up, 11.0 months; median follow-up, 24.4 months [nivolumab] and 22.5 months [placebo]) and patients with PD-L1 ≥1% (minimum follow-up, 11.4 months; median follow-up, 25.5 months [nivolumab] and 22.4 months [placebo]; Table). DFS probability at 12 months was 63.5% with nivolumab and 46.9% with placebo in ITT patients. Among patients with PD-L1 ≥1%, DFS probability at 12 months was 67.6% with nivolumab and 46.3% with placebo. Improvement in DFS was observed with nivolumab versus placebo for most subgroups analyzed, including age, sex, ECOG PS, nodal status, use of prior cisplatin-based chemotherapy, and PD-L1 status. NUTRFS and DMFS were also improved with nivolumab versus placebo in both ITT patients and those with PD-L1 ≥1% (Table).
Conclusions:
With longer follow-up, nivolumab continued to demonstrate clinically meaningful improvement in DFS versus placebo for patients with high-risk MIUC after radical surgery, both in ITT patients and in patients with PD-L1 ≥1%. DFS benefit was observed in most prespecified subgroups. NUTRFS and DMFS were also improved with nivolumab compared with placebo in both ITT patients and those with PD-L1 ≥1%. These results support adjuvant nivolumab as a standard-of-care treatment for patients with high-risk MIUC after radical surgery.
Table
JL1007E Table
To view the table, please click on this link from the e-poster gallery on jadprolive.com

