Back
Industry Encore Posters
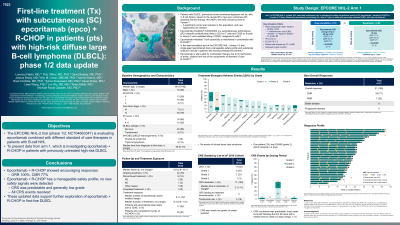
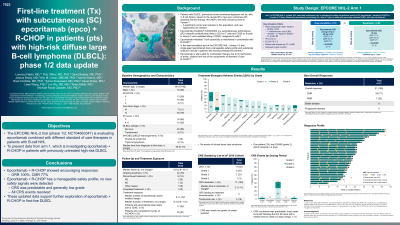
JL1014E: First-line treatment (Tx) with subcutaneous (SC) epcoritamab (epco) + R-CHOP in patients (pts) with high-risk diffuse large B-cell lymphoma (DLBCL): phase 1/2 data update
Saturday, October 22, 2022
10:00 AM – 11:00 AM ET

Landon Shupe, PharmD
Medical Science Liaison
Genmab US, Inc.
Poster Presenter(s)
Background:
Outcomes of pts with newly diagnosed DLBCL with high/poor risk according to the revised International Prognostic Index (IPI) treated with immunochemotherapy (IC) remain suboptimal, with a 4-year survival rate of 55% (Sehn et al, Blood 2007). SC epco is a well-tolerated bispecific antibody with single-agent activity in the relapsed/refractory (R/R) aggressive B-cell NHL setting. The mechanism of action and safety profile of epco are distinct from IC, and epco is well suited for use in combinations and in earlier lines of therapy. Addition of a novel agent to standard of care IC may overcome the adverse prognosis of high-risk pts. Presented here are updated results of epco + rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) in previously untreated DLBCL pts with IPI 3–5 (EPCORE NHL-2 arm 1; NCT04663347).
Methods:
Adults with previously untreated CD20+ DLBCL and IPI ≥3 received SC epco (every week, cycle [C] 1–4; every 3 weeks, C5–6) + R-CHOP for 6 cycles (21 d) followed by single-agent epco every 4 weeks up to 1 y (in cycles of 28 d). To mitigate CRS, epco step-up dosing and corticosteroid prophylaxis were required. Response was assessed by PET-CT with contrast per Lugano 2014 criteria.
Results:
As of Dec 1, 2021, 33 pts (median age, 66 y; range, 19–82) received epco + R-CHOP (epco 24 mg, n=4; 48 mg, n=29). Median time from diagnosis to first dose was 25 d (range, 5–70). All pts had IPI ≥3 and ≥24% had double- or triple-hit DLBCL. Median follow-up was 3 mo (range, 0–9.7); median number of total cycles initiated was 5 (1–13). Overall, 94% of pts (31/33) remained on Tx. Tx-emergent adverse events (TEAEs) in ≥30% of pts were neutropenia (48%; febrile neutropenia in 9% of all pts), CRS (45%), infections (42%), anemia (39%), injection-site reactions (36%), nausea (33%), constipation (30%), and pyrexia (30%). No TEAEs led to epco discontinuation. AEs of special interest included CRS (42% grade [G] 1/2, 3% G3) and ICANS (3% G2); 1 pt had tumor lysis syndrome (3% G3). Most CRS events occurred in C1 and resolved after a median of 2 days (1–11); 4 pts with CRS received tocilizumab. No fatal TEAEs were reported. In efficacy-evaluable pts, the overall response rate (ORR) was 96% (24/25); 68% (17/25) had complete metabolic response (CMR). For the 10 pts who received 6 cycles of R-CHOP and had a subsequent response assessment, the ORR and CMR rate were 100% and 90%, respectively. As of the data cutoff, all of these 10 pts remained in response, with the longest duration of response 7.1+ mo and ongoing. Updated data will be presented.
Conclusions:
Epco is the first SC bispecific antibody assessed in combination with standard of care in previously untreated DLBCL. The safety profile of epco + R-CHOP is manageable. CRS events were mostly of low grade and did not lead to Tx discontinuation. ORR and CMR rate were high with no relapses as of the data cutoff date.
Outcomes of pts with newly diagnosed DLBCL with high/poor risk according to the revised International Prognostic Index (IPI) treated with immunochemotherapy (IC) remain suboptimal, with a 4-year survival rate of 55% (Sehn et al, Blood 2007). SC epco is a well-tolerated bispecific antibody with single-agent activity in the relapsed/refractory (R/R) aggressive B-cell NHL setting. The mechanism of action and safety profile of epco are distinct from IC, and epco is well suited for use in combinations and in earlier lines of therapy. Addition of a novel agent to standard of care IC may overcome the adverse prognosis of high-risk pts. Presented here are updated results of epco + rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) in previously untreated DLBCL pts with IPI 3–5 (EPCORE NHL-2 arm 1; NCT04663347).
Methods:
Adults with previously untreated CD20+ DLBCL and IPI ≥3 received SC epco (every week, cycle [C] 1–4; every 3 weeks, C5–6) + R-CHOP for 6 cycles (21 d) followed by single-agent epco every 4 weeks up to 1 y (in cycles of 28 d). To mitigate CRS, epco step-up dosing and corticosteroid prophylaxis were required. Response was assessed by PET-CT with contrast per Lugano 2014 criteria.
Results:
As of Dec 1, 2021, 33 pts (median age, 66 y; range, 19–82) received epco + R-CHOP (epco 24 mg, n=4; 48 mg, n=29). Median time from diagnosis to first dose was 25 d (range, 5–70). All pts had IPI ≥3 and ≥24% had double- or triple-hit DLBCL. Median follow-up was 3 mo (range, 0–9.7); median number of total cycles initiated was 5 (1–13). Overall, 94% of pts (31/33) remained on Tx. Tx-emergent adverse events (TEAEs) in ≥30% of pts were neutropenia (48%; febrile neutropenia in 9% of all pts), CRS (45%), infections (42%), anemia (39%), injection-site reactions (36%), nausea (33%), constipation (30%), and pyrexia (30%). No TEAEs led to epco discontinuation. AEs of special interest included CRS (42% grade [G] 1/2, 3% G3) and ICANS (3% G2); 1 pt had tumor lysis syndrome (3% G3). Most CRS events occurred in C1 and resolved after a median of 2 days (1–11); 4 pts with CRS received tocilizumab. No fatal TEAEs were reported. In efficacy-evaluable pts, the overall response rate (ORR) was 96% (24/25); 68% (17/25) had complete metabolic response (CMR). For the 10 pts who received 6 cycles of R-CHOP and had a subsequent response assessment, the ORR and CMR rate were 100% and 90%, respectively. As of the data cutoff, all of these 10 pts remained in response, with the longest duration of response 7.1+ mo and ongoing. Updated data will be presented.
Conclusions:
Epco is the first SC bispecific antibody assessed in combination with standard of care in previously untreated DLBCL. The safety profile of epco + R-CHOP is manageable. CRS events were mostly of low grade and did not lead to Tx discontinuation. ORR and CMR rate were high with no relapses as of the data cutoff date.