Back
Industry Encore Posters
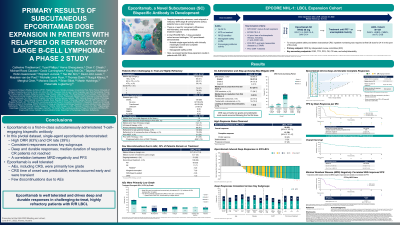
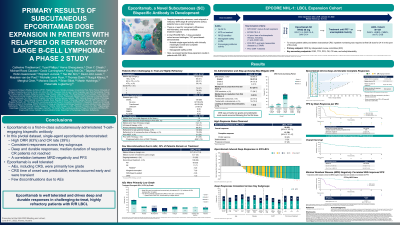
JL1028E: PRIMARY RESULTS OF SUBCUTANEOUS EPCORITAMAB DOSE EXPANSION IN PATIENTS WITH RELAPSED OR REFRACTORY LARGE B-CELL LYMPHOMA: A PHASE 2 STUDY
Saturday, October 22, 2022
10:00 AM – 11:00 AM ET

Landon Shupe, PharmD
Medical Science Liaison
Genmab US, Inc.
Poster Presenter(s)
Background:
Recently, multiple therapies have emerged with novel mechanisms of action, but an unmet need remains for more tolerable and readily available treatment options that can induce deep and durable responses in patients (pts) with relapsed or refractory (R/R) large B-cell lymphoma (LBCL). Epcoritamab is a novel, subcutaneous (SC) CD3/CD20 bispecific antibody that has shown preliminary potent antitumor activity across B-cell NHL subtypes in dose escalation as a single agent and in combination with various standards of care.
Aims:
We report primary results from the LBCL expansion cohort in the phase 2 study of SC epcoritamab in pts with R/R B-cell NHL (EPCORE NHL-1; NCT03625037).
Methods:
Adults with R/R CD20+ LBCL received epcoritamab (priming and intermediate doses followed by full doses of 48 mg) as 1-mL SC injections in cycles (C) of 28 days (QW: C1–3; Q2W: C4–9; Q4W C≥10) until disease progression or unacceptable toxicity. CRS mitigation included step-up dosing and corticosteroid prophylaxis (C1 only). Per protocol, 24-h hospitalization was only required for the first full dose to ensure close observation of the pts. Informed consent was obtained.
Results:
As of Jan 31, 2022, 157 pts with DLBCL (including double/triple-hit and transformed), high-grade B-cell lymphoma (HGBCL), primary mediastinal LBCL (PMBCL), or follicular lymphoma (FL) grade 3B were treated. Median age was 64 y (range, 20–83) with 49.0% ≥65 y and 18.5% ≥75 y. Pts had a median of 3 (range, 2–11) prior lines of therapy (LOT), and a median of 1.6 y from initial diagnosis. Notably, 61 pts (38.9%) received prior CAR T (75% of those progressed within 6 mo of CAR T) and 31 (19.7%) had prior ASCT (58% of those progressed within 12 mo of ASCT). Overall, 61% had primary refractory disease, and 83% were refractory to the last LOT. At a median follow-up of 10.7 mo, the overall response rate (ORR) by IRC based on Lugano criteria and assessed by PET-CT was 63% with 39% complete response (CR); see Figure. The ORR/CR rates were 69%/42% for CAR T–naive pts and 54%/34% for pts with prior CAR T. The median duration of response (mDOR) was 12 mo, while the mDOR among pts achieving CR was not reached, with 89% still in CR at 9 mo (KM estimate). ORR was similar across prespecified subgroups of age, prior LOT, and de novo or transformed disease. The most common treatment-emergent AEs (TEAEs) of any grade were cytokine release syndrome (CRS; 49.7%), pyrexia (23.6%), fatigue (22.9%), neutropenia (21.7%), and diarrhea (20.4%). Twelve pts (7.6%) had TEAEs that led to treatment discontinuation; 3 were considered treatment related (CRS, worsening CLIPPERS, and ICANS). Incidence of CRS events was: G1 31.8%, G2 15.3%, and G3 2.5%; events occurred mainly following the first full dose on C1D15 (median onset 20 h after SC injection; median time to resolution 48 h). Overall, 22 pts (14%) received tocilizumab. Ten pts (6.4%) experienced ICANS; all but one event was G1/2, and G5 ICANS was the only treatment-related death.
Conclusion/Summary:
Epcoritamab is a convenient, SC, off-the-shelf therapy that demonstrated clinically meaningful and compelling efficacy including deep and durable responses in a challenging to treat, highly refractory LBCL population. While efficacy was observed in both CAR T–exposed and CAR T–naive pts, a numerically higher percentage of CAR T–naive pts responded to single-agent epcoritamab. The safety profile was manageable and consistent with previous findings. Notably, most CRS events were low grade and occurred during C1, ICANS was limited, and there were few discontinuations due to AEs.
This abstract was accepted and presented at the European Hematology Association (EHA) 2022 30th Annual Congress, June 9-12, 2022 in Vienna, Austria.
Recently, multiple therapies have emerged with novel mechanisms of action, but an unmet need remains for more tolerable and readily available treatment options that can induce deep and durable responses in patients (pts) with relapsed or refractory (R/R) large B-cell lymphoma (LBCL). Epcoritamab is a novel, subcutaneous (SC) CD3/CD20 bispecific antibody that has shown preliminary potent antitumor activity across B-cell NHL subtypes in dose escalation as a single agent and in combination with various standards of care.
Aims:
We report primary results from the LBCL expansion cohort in the phase 2 study of SC epcoritamab in pts with R/R B-cell NHL (EPCORE NHL-1; NCT03625037).
Methods:
Adults with R/R CD20+ LBCL received epcoritamab (priming and intermediate doses followed by full doses of 48 mg) as 1-mL SC injections in cycles (C) of 28 days (QW: C1–3; Q2W: C4–9; Q4W C≥10) until disease progression or unacceptable toxicity. CRS mitigation included step-up dosing and corticosteroid prophylaxis (C1 only). Per protocol, 24-h hospitalization was only required for the first full dose to ensure close observation of the pts. Informed consent was obtained.
Results:
As of Jan 31, 2022, 157 pts with DLBCL (including double/triple-hit and transformed), high-grade B-cell lymphoma (HGBCL), primary mediastinal LBCL (PMBCL), or follicular lymphoma (FL) grade 3B were treated. Median age was 64 y (range, 20–83) with 49.0% ≥65 y and 18.5% ≥75 y. Pts had a median of 3 (range, 2–11) prior lines of therapy (LOT), and a median of 1.6 y from initial diagnosis. Notably, 61 pts (38.9%) received prior CAR T (75% of those progressed within 6 mo of CAR T) and 31 (19.7%) had prior ASCT (58% of those progressed within 12 mo of ASCT). Overall, 61% had primary refractory disease, and 83% were refractory to the last LOT. At a median follow-up of 10.7 mo, the overall response rate (ORR) by IRC based on Lugano criteria and assessed by PET-CT was 63% with 39% complete response (CR); see Figure. The ORR/CR rates were 69%/42% for CAR T–naive pts and 54%/34% for pts with prior CAR T. The median duration of response (mDOR) was 12 mo, while the mDOR among pts achieving CR was not reached, with 89% still in CR at 9 mo (KM estimate). ORR was similar across prespecified subgroups of age, prior LOT, and de novo or transformed disease. The most common treatment-emergent AEs (TEAEs) of any grade were cytokine release syndrome (CRS; 49.7%), pyrexia (23.6%), fatigue (22.9%), neutropenia (21.7%), and diarrhea (20.4%). Twelve pts (7.6%) had TEAEs that led to treatment discontinuation; 3 were considered treatment related (CRS, worsening CLIPPERS, and ICANS). Incidence of CRS events was: G1 31.8%, G2 15.3%, and G3 2.5%; events occurred mainly following the first full dose on C1D15 (median onset 20 h after SC injection; median time to resolution 48 h). Overall, 22 pts (14%) received tocilizumab. Ten pts (6.4%) experienced ICANS; all but one event was G1/2, and G5 ICANS was the only treatment-related death.
Conclusion/Summary:
Epcoritamab is a convenient, SC, off-the-shelf therapy that demonstrated clinically meaningful and compelling efficacy including deep and durable responses in a challenging to treat, highly refractory LBCL population. While efficacy was observed in both CAR T–exposed and CAR T–naive pts, a numerically higher percentage of CAR T–naive pts responded to single-agent epcoritamab. The safety profile was manageable and consistent with previous findings. Notably, most CRS events were low grade and occurred during C1, ICANS was limited, and there were few discontinuations due to AEs.
This abstract was accepted and presented at the European Hematology Association (EHA) 2022 30th Annual Congress, June 9-12, 2022 in Vienna, Austria.

