Back

APSHO Patient Perspective Posters
JL1005P: Complex Biomarker Reports Suggest Need for Patient-Friendly Reporting and Education
Saturday, October 22, 2022
10:00 AM – 11:00 AM ET
Has Audio

Nikki Martin, MA (she/her/hers)
Senior Director, Precision Medicine Initiatives
LUNGevity Foundation
Poster Presenter(s)
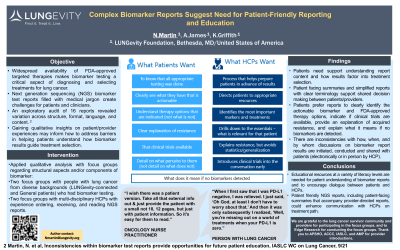
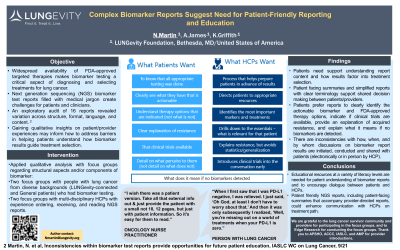
Background:
The widespread availability of FDA-approved targeted therapies makes biomarker testing a critical aspect of diagnosing lung cancer, informing treatment selection and patient outcomes. However, complex next generation sequencing (NGS) biomarker test reports filled with medical jargon create challenges for patients and clinicians, generating patient confusion and anxiety. An exploratory audit of 12 commercial laboratory NGS results reports and 4 academic NGS reports revealed variation across NGS reports in terms of structure, format, language, and content.Gaining qualitative insights on patient and provider experiences with biomarker testing, results reporting, and discussion of biomarker test findings may highlight additional unmet needs and facilitate a greater understanding of how to address barriers in helping patients understand how biomarker results guide treatment decisions.
Intervention:
Using qualitative analysis, structural aspects and/or components of biomarker reports were reported as confusing or frequently misunderstood by patients and providers. Two focus groups were conducted with lung cancer patients who had undergone biomarker testing. One patient group was sourced from the LUNGevity network, and the other group consisted of patients with no connection to LUNGevity. In addition, two discussion groups with multi-disciplinary healthcare providers (HCPs) focused on their experience with ordering, receiving, and reading NGS reports, typical patient interaction on biomarker results, and need for patient education.
Findings:
Results indicated a broad spectrum of patient experiences regarding biomarker test results reports with a pronounced need for assisting patients with understanding report content. Physicians recognized this need and shared their personal challenges with accessing and interpretation of the reports. Both groups agreed that simple, easy-to-access reports with clear terminology and patient-friendly summaries would benefit the lung cancer community. More specifically, the study revealed inconsistencies related to: 1) how, when, and by whom discussions on biomarker report results are initiated and conducted; 2) the delivery of the report results to the patient (electronically from the hospital or lab or in person by HCP); and 3) how the biomarker test results factor into treatment selection. Patients expressed a preference for reports to clearly identify the actionable biomarker and FDA-approved therapy options, indicate if clinical trials are available, provide an explanation of acquired resistance, and explain what it means if no biomarkers are detected.
Implications:
Based on these findings, LUNGevity is working with the Association of Community Cancer Centers, Association for Molecular Pathology, Advanced Practitioner Society of Hematology and Oncology, and the International Association for the Study of Lung Cancer to create comprehensive and health literate educational resources designed to facilitate patient understanding of biomarker reports and to encourage dialogue between patients and their healthcare team. The findings are the basis for ongoing conversations with laboratories for more patient focused NGS reports, including creating patient-facing summaries that accompany provider-directed reports, and simplification to support patient-provider shared decision making in treatment.
The widespread availability of FDA-approved targeted therapies makes biomarker testing a critical aspect of diagnosing lung cancer, informing treatment selection and patient outcomes. However, complex next generation sequencing (NGS) biomarker test reports filled with medical jargon create challenges for patients and clinicians, generating patient confusion and anxiety. An exploratory audit of 12 commercial laboratory NGS results reports and 4 academic NGS reports revealed variation across NGS reports in terms of structure, format, language, and content.Gaining qualitative insights on patient and provider experiences with biomarker testing, results reporting, and discussion of biomarker test findings may highlight additional unmet needs and facilitate a greater understanding of how to address barriers in helping patients understand how biomarker results guide treatment decisions.
Intervention:
Using qualitative analysis, structural aspects and/or components of biomarker reports were reported as confusing or frequently misunderstood by patients and providers. Two focus groups were conducted with lung cancer patients who had undergone biomarker testing. One patient group was sourced from the LUNGevity network, and the other group consisted of patients with no connection to LUNGevity. In addition, two discussion groups with multi-disciplinary healthcare providers (HCPs) focused on their experience with ordering, receiving, and reading NGS reports, typical patient interaction on biomarker results, and need for patient education.
Findings:
Results indicated a broad spectrum of patient experiences regarding biomarker test results reports with a pronounced need for assisting patients with understanding report content. Physicians recognized this need and shared their personal challenges with accessing and interpretation of the reports. Both groups agreed that simple, easy-to-access reports with clear terminology and patient-friendly summaries would benefit the lung cancer community. More specifically, the study revealed inconsistencies related to: 1) how, when, and by whom discussions on biomarker report results are initiated and conducted; 2) the delivery of the report results to the patient (electronically from the hospital or lab or in person by HCP); and 3) how the biomarker test results factor into treatment selection. Patients expressed a preference for reports to clearly identify the actionable biomarker and FDA-approved therapy options, indicate if clinical trials are available, provide an explanation of acquired resistance, and explain what it means if no biomarkers are detected.
Implications:
Based on these findings, LUNGevity is working with the Association of Community Cancer Centers, Association for Molecular Pathology, Advanced Practitioner Society of Hematology and Oncology, and the International Association for the Study of Lung Cancer to create comprehensive and health literate educational resources designed to facilitate patient understanding of biomarker reports and to encourage dialogue between patients and their healthcare team. The findings are the basis for ongoing conversations with laboratories for more patient focused NGS reports, including creating patient-facing summaries that accompany provider-directed reports, and simplification to support patient-provider shared decision making in treatment.

