Back
Therapeutics- Local (Primary and Metastases)
28: Treatment decisions among patients newly diagnosed with clinical T1 renal masses
Location: Poster Hall, Board C4
Width: 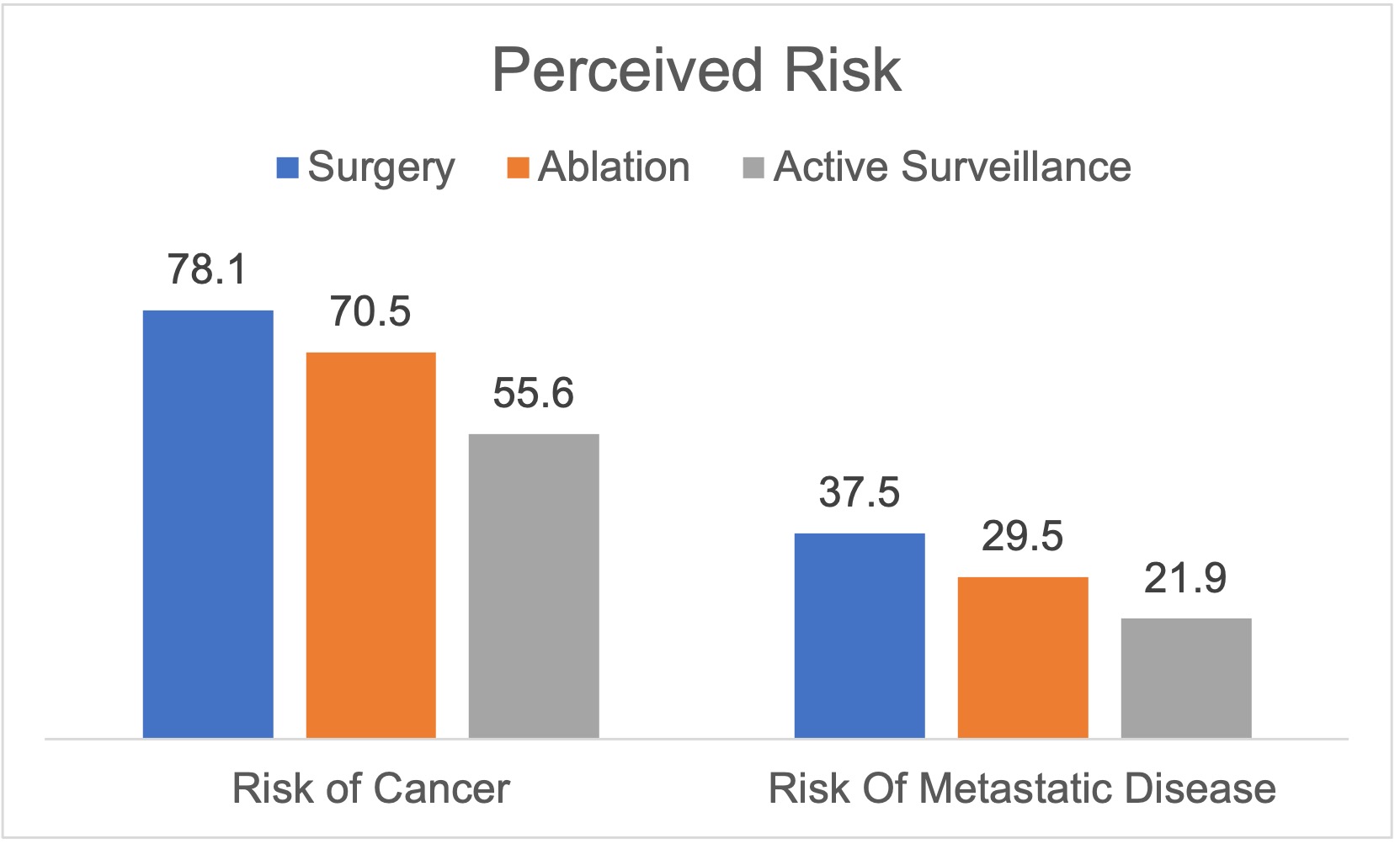
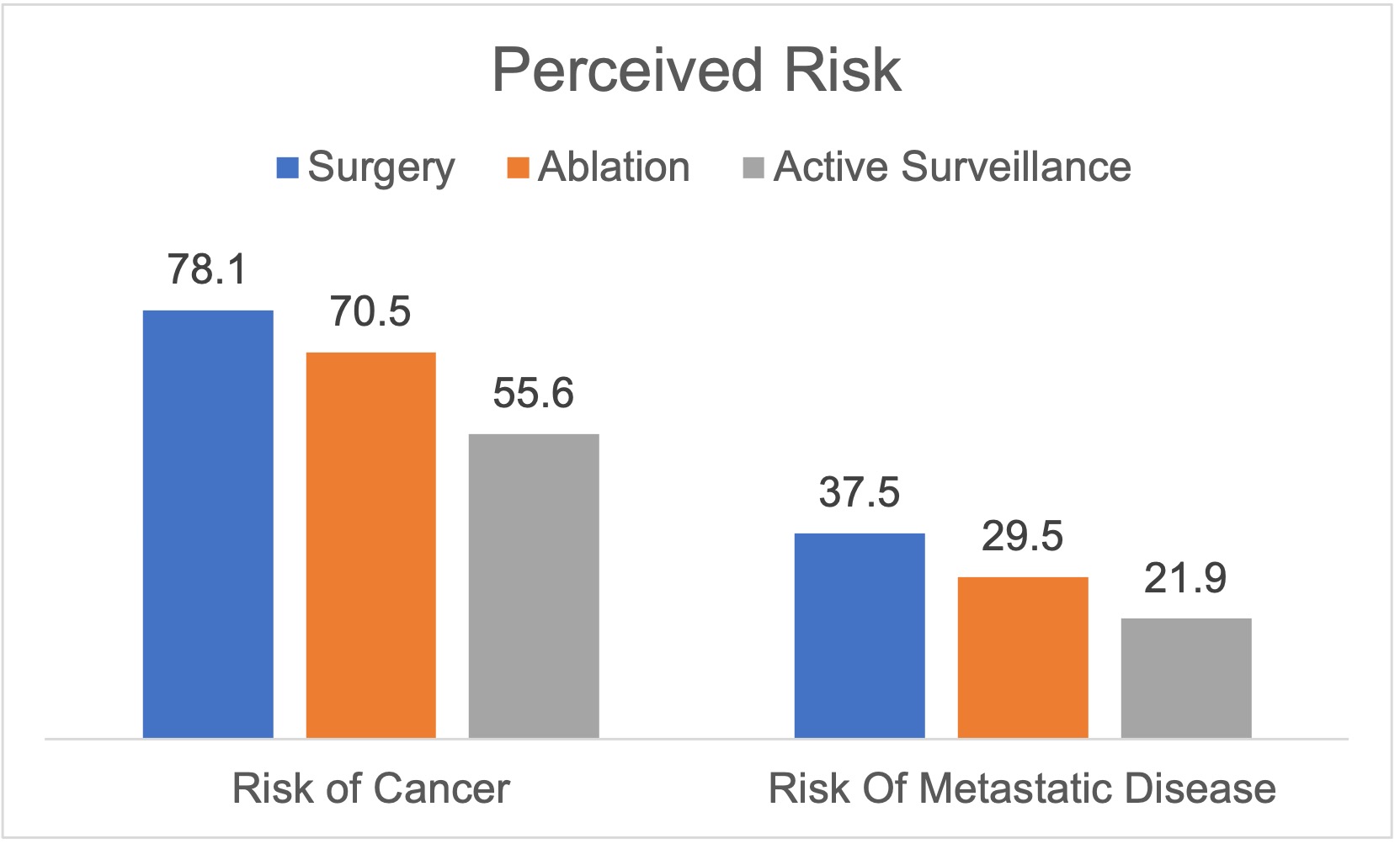
Figure. Perceived risk of cancer and metastatic disease by treatment decision.
- KG
Kathryn H. Gessner, MD, PhD
Clinical Fellow
University of North Carolina at Chapel Hill, United States
Poster Presenter(s)
Background: Patients with clinical T1 renal masses face an increasingly complex decision given the multitude of available management options. In this study, we evaluate clinical, tumor, and decision-making factors driving treatment selection among patients with clinical T1 renal masses.
Methods: From October 2018–June 2022, we enrolled patients with new clinical T1 renal masses onto GRADE-SRM (Genomic Risk Assessment and Decisional Evaluation for Small Renal Masses), a comparative, non-randomized hybrid trial investigating the decision-making experience and cancer genomics. At study entry, participants completed a baseline survey to characterize decision-making, communication, demographic characteristics, health status, tumor burden, and perceived risk of cancer presence and metastatic potential. Treatment decision served as the primary outcome defined as surgery, ablation, and active surveillance. We compared treatment decision by patient and tumor characteristics using bivariable analyses.
Results: For 245 subjects, 59% selected surgery, 34% opted for active surveillance, and 5% chose ablation. Treatment decisions varied by age (p < 0.001), gender (p=0.015), performance status (p < 0.001), comorbidity (p < 0.001), cardiac history (p=0.008), eGFR (p=0.007), mass size (p < 0.001), nephrometry score (p=0.001), and solid vs. cystic mass (p < 0.001). Treatment decisions further related to information-seeking behavior (p=0.020), decisional conflict (p=0.040), and cancer worry (p=0.004). Subjects selecting active surveillance perceived cancer and metastasis risks to be lower than subjects choosing surgery/ablation (Figure). Renal mass biopsy was also associated with decisions for surgery or ablation (p=0.020).
Conclusions: In patients with clinical T1 renal masses, treatment decisions differed based on patient health and tumor characteristics, likely in response to potential risks and benefits for management options. Beyond these less modifiable factors, treatment decisions also differed based on patient risk perception, information processing, and decision-making behavior. These relationships highlight the opportunity for communication frameworks and prognostic biomarkers to further improve the patient decision-making experience.
Methods: From October 2018–June 2022, we enrolled patients with new clinical T1 renal masses onto GRADE-SRM (Genomic Risk Assessment and Decisional Evaluation for Small Renal Masses), a comparative, non-randomized hybrid trial investigating the decision-making experience and cancer genomics. At study entry, participants completed a baseline survey to characterize decision-making, communication, demographic characteristics, health status, tumor burden, and perceived risk of cancer presence and metastatic potential. Treatment decision served as the primary outcome defined as surgery, ablation, and active surveillance. We compared treatment decision by patient and tumor characteristics using bivariable analyses.
Results: For 245 subjects, 59% selected surgery, 34% opted for active surveillance, and 5% chose ablation. Treatment decisions varied by age (p < 0.001), gender (p=0.015), performance status (p < 0.001), comorbidity (p < 0.001), cardiac history (p=0.008), eGFR (p=0.007), mass size (p < 0.001), nephrometry score (p=0.001), and solid vs. cystic mass (p < 0.001). Treatment decisions further related to information-seeking behavior (p=0.020), decisional conflict (p=0.040), and cancer worry (p=0.004). Subjects selecting active surveillance perceived cancer and metastasis risks to be lower than subjects choosing surgery/ablation (Figure). Renal mass biopsy was also associated with decisions for surgery or ablation (p=0.020).
Conclusions: In patients with clinical T1 renal masses, treatment decisions differed based on patient health and tumor characteristics, likely in response to potential risks and benefits for management options. Beyond these less modifiable factors, treatment decisions also differed based on patient risk perception, information processing, and decision-making behavior. These relationships highlight the opportunity for communication frameworks and prognostic biomarkers to further improve the patient decision-making experience.
