Back
Quality of Care and Quality Improvement
18: Non-Index vs Index Readmissions Following Radical Nephrectomy: Causes, Costs, and Outcomes
Location: Poster Hall, Board B2
Width: 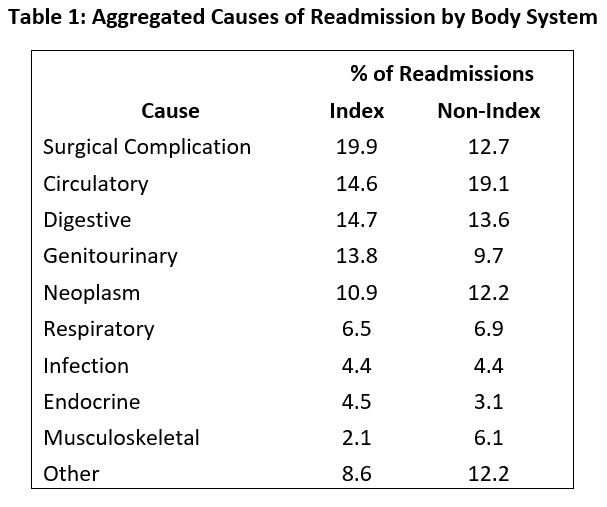
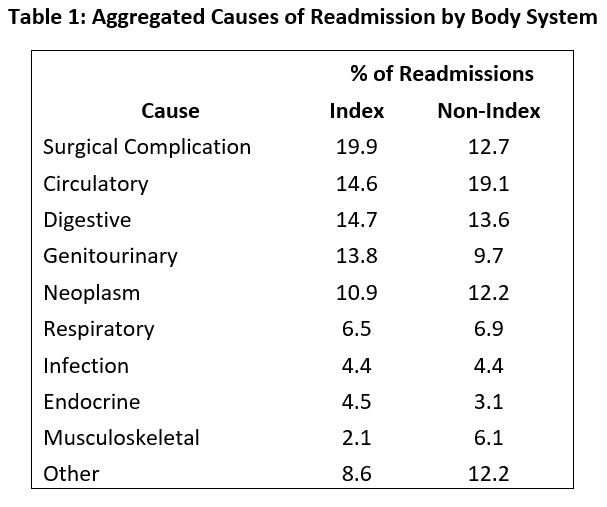
Table 1: Aggregated Causes of Readmission by Body System

Shiva Balasubramanian, B.A.
MS3
University of Missouri-Kansas City School of Medicine, United States
Poster Presenter(s)
Background: Readmission in the 90-day postoperative period represents a considerable burden on patients and hospitals. Non-index readmissions are especially burdensome as they may represent care fragmentation. Using the 2010-2014 Nationwide Readmissions Databases (NRD), we aimed to describe and compare index and non-index readmissions following radical nephrectomy for treating malignant renal neoplasms.
Methods: Patients with malignant renal neoplasms that underwent radical nephrectomy were identified and abstracted using International Classification of Diseases-9 coding. Differences in readmission-visit outcomes between index and non-index readmissions were assessed using the χ2 test. Statistical significance was defined as p< 0.05.
Results: Of 26,794 patients that underwent a radical nephrectomy, 2,620 (9.8%) were readmitted within 90-days. Index hospital readmissions accounted for 1,826/2,620 (69.7%) readmissions and non-index hospital readmissions accounted for 794/2,620 (30.3%) readmissions. The most prevalent cause of index readmission was surgical complication accounting for 363/1,826 (19.9%) index readmissions; the most prevalent cause of non-index readmission was circulatory system pathology accounting for 151/794 (19.1%) non-index readmissions. Mean cost of a non-index readmission was $12,829±342, which was significantly lower than the mean cost of an index readmission – $13,292±319 (p < 0.01). In terms of readmission visit discharge disposition, a higher proportion of non-index readmission patients received a non-routine discharge (30% vs 23%, p=0.039). Non-index readmissions had a significantly higher mortality rate compared to index readmissions, (3.7% vs 1.1%, p< 0.01).
Conclusions: Non-index readmissions account for nearly one third of readmissions following radical nephrectomy to treat malignant renal neoplasms and have a higher mortality rate than index readmissions. A better understanding of non-index readmissions allows for the development of targeted interventions aimed at reducing these occurrences, thereby preventing fragmentation of care.
Methods: Patients with malignant renal neoplasms that underwent radical nephrectomy were identified and abstracted using International Classification of Diseases-9 coding. Differences in readmission-visit outcomes between index and non-index readmissions were assessed using the χ2 test. Statistical significance was defined as p< 0.05.
Results: Of 26,794 patients that underwent a radical nephrectomy, 2,620 (9.8%) were readmitted within 90-days. Index hospital readmissions accounted for 1,826/2,620 (69.7%) readmissions and non-index hospital readmissions accounted for 794/2,620 (30.3%) readmissions. The most prevalent cause of index readmission was surgical complication accounting for 363/1,826 (19.9%) index readmissions; the most prevalent cause of non-index readmission was circulatory system pathology accounting for 151/794 (19.1%) non-index readmissions. Mean cost of a non-index readmission was $12,829±342, which was significantly lower than the mean cost of an index readmission – $13,292±319 (p < 0.01). In terms of readmission visit discharge disposition, a higher proportion of non-index readmission patients received a non-routine discharge (30% vs 23%, p=0.039). Non-index readmissions had a significantly higher mortality rate compared to index readmissions, (3.7% vs 1.1%, p< 0.01).
Conclusions: Non-index readmissions account for nearly one third of readmissions following radical nephrectomy to treat malignant renal neoplasms and have a higher mortality rate than index readmissions. A better understanding of non-index readmissions allows for the development of targeted interventions aimed at reducing these occurrences, thereby preventing fragmentation of care.
