Back
Women's Mental Health
Poster Session
(202) Psychiatry's Role in Caring for Patient Survivors of Female Genital Mutilation
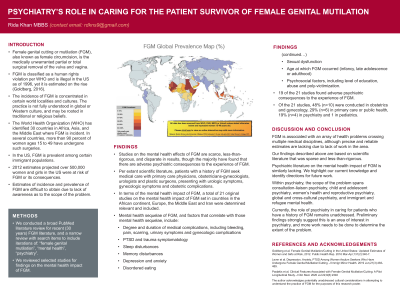
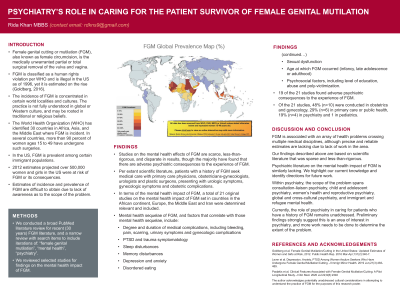
Abstract: Background/Significance: Female genital mutilation (FGM) is the medically unwarranted partial or total surgical removal of the vulva and vagina. FGM is a human rights violation per WHO and is prohibited by law in the US, yet prevalence is estimated on the rise (Goldberg, 2016). Per extant scientific literature, patient survivors of FGM seek medical care with primary care physicians, obstetricians-gynecologists, urologists and plastic surgeons. Psychiatric literature on the mental health impact of FGM is lacking.
Methods: We conducted a broad PubMed literature search for recent (20 years) FGM literature yielding 2,938 results and reviewed studies for findings on the mental health impact of FGM.
Results: Studies on the mental health effects of FGM were scarce, less-than-rigorous and disparate in results. A total of 21 original studies addressing the mental health impact of FGM set in countries in the African continent, Europe, the Middle East, Iran and the USA were determined relevant and included. Collating reported findings, psychiatric sequelae of FGM include depression, anxiety, PTSD, disordered eating, memory issues, and sleep problems. Psychiatric symptoms were studied in correlation with degree and duration of medical complications (including bleeding, pain, scarring), urologic, gynecologic, obstetric, antenatal and postnatal complications, sexual function, surgical intervention, age at which FGM occurred (infancy, late adolescence or adulthood) and social factors such as level of education and environment (abuse and polyvictimization). 19 of 21 studies found adverse psychiatric consequences to the experience of FGM. Of the 21 studies, 48% (n=10) were conducted in obstetrics and gynecology, 29% (n=6) in primary care or public health, 19% (n=4) in psychiatry and 1 in pediatrics.
Discussion: Though FGM is associated with a complex array of health problems crossing multiple medical disciplines, it is a neglected area of study and work. Within psychiatry, the scope of the problem spans consultation/liaison psychiatry, child and adolescent psychiatry, women’s mental health and reproductive psychiatry, global and cross-cultural psychiatry, and immigrant and refugee mental health.
Conclusion/Implications: The medical management of FGM is complex and multidisciplinary, yet work in the area is severely lacking. The role of psychiatry in caring for patients with FGM has not been addressed. Preliminary findings strongly suggest this is an area of interest in psychiatry and more work needs to be done to determine the scope of the problem.
References:
- Goldberg et al. Female Genital Mutilation/Cutting in the United States: Updated Estimates of Women and Girls at Risk, 2012. Public Health Rep. 2016 Mar-Apr;131(2):340-7.
- Lever et al. Depression, Anxiety, PTSD Among Women Asylum Seekers Who Have Undergone Female Genital Mutilation/Cutting. J Immigr Minor Health. 2019 Jun;21(3):483-489.
- Paslakis et al. Clinical Features Associated with Female Genital Mutilation/Cutting: A Pilot Longitudinal Study. J Clin Med. 2020 Jul 22;9(8):2340
Methods: We conducted a broad PubMed literature search for recent (20 years) FGM literature yielding 2,938 results and reviewed studies for findings on the mental health impact of FGM.
Results: Studies on the mental health effects of FGM were scarce, less-than-rigorous and disparate in results. A total of 21 original studies addressing the mental health impact of FGM set in countries in the African continent, Europe, the Middle East, Iran and the USA were determined relevant and included. Collating reported findings, psychiatric sequelae of FGM include depression, anxiety, PTSD, disordered eating, memory issues, and sleep problems. Psychiatric symptoms were studied in correlation with degree and duration of medical complications (including bleeding, pain, scarring), urologic, gynecologic, obstetric, antenatal and postnatal complications, sexual function, surgical intervention, age at which FGM occurred (infancy, late adolescence or adulthood) and social factors such as level of education and environment (abuse and polyvictimization). 19 of 21 studies found adverse psychiatric consequences to the experience of FGM. Of the 21 studies, 48% (n=10) were conducted in obstetrics and gynecology, 29% (n=6) in primary care or public health, 19% (n=4) in psychiatry and 1 in pediatrics.
Discussion: Though FGM is associated with a complex array of health problems crossing multiple medical disciplines, it is a neglected area of study and work. Within psychiatry, the scope of the problem spans consultation/liaison psychiatry, child and adolescent psychiatry, women’s mental health and reproductive psychiatry, global and cross-cultural psychiatry, and immigrant and refugee mental health.
Conclusion/Implications: The medical management of FGM is complex and multidisciplinary, yet work in the area is severely lacking. The role of psychiatry in caring for patients with FGM has not been addressed. Preliminary findings strongly suggest this is an area of interest in psychiatry and more work needs to be done to determine the scope of the problem.
References:
- Goldberg et al. Female Genital Mutilation/Cutting in the United States: Updated Estimates of Women and Girls at Risk, 2012. Public Health Rep. 2016 Mar-Apr;131(2):340-7.
- Lever et al. Depression, Anxiety, PTSD Among Women Asylum Seekers Who Have Undergone Female Genital Mutilation/Cutting. J Immigr Minor Health. 2019 Jun;21(3):483-489.
- Paslakis et al. Clinical Features Associated with Female Genital Mutilation/Cutting: A Pilot Longitudinal Study. J Clin Med. 2020 Jul 22;9(8):2340

Rida Khan, MBBS (she/her/hers)
N/A
N/A, MN, United States