Back
Collaborative and Integrated Care
Poster Session
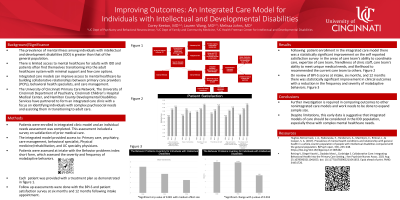
(018) Improving Outcomes: An Integrated Care Model for Individuals with Intellectual and Developmental Disabilities
Abstract: Improving Outcomes: An Integrated Care Model for Individuals with Intellectual and Developmental Disabilities
Background/Significance: The prevalence of mental illness among individuals with intellectual and developmental disabilities is greater than that of the general population. There is limited access to mental healthcare for adults with IDD in most communities. Patients often find themselves transitioning into the adult healthcare system with minimal support and few care options. The use of integrated care models can improve access to mental health care by building collaborative relationships between primary care providers, behavioral health specialists, and care management.
Methods: The University of Cincinnati Primary Care Network, The University of Cincinnati Department of Psychiatry, Cincinnati Children’s Hospital Medical Center, and Hamilton County Developmental Disabilities Services have partnered to form one such integrated care clinic. The focus is to identify individuals with complex psychosocial needs and to assist them in transitioning to adult care. In having an integrated care model where patients with IDD are able to obtain preventative medical care, acute medical care, psychiatric services, and support services there is expected to be overall improvement in patient/caregiver satisfaction and in clinical outcomes. Patient satisfaction scores was monitored via patient/caregiver surveys at the time of establishment in the integrated clinic, at six months, and at twelve months. Surveys were done looking at clinical outcomes. The Behavior Problem Inventory for Intellectual Disabilities Short Form was given at the same intervals to monitor changes in the frequently and severity of identified maladaptive behaviors.
Results: Following implementation of the integrated care model there was statistically significant improvement in patient satisfaction. Specifically there was improvement noted in the areas of care teams ability to meet unique needs, medical expertise of care team, and the collaboration between care team members. There was also statistically significant improvement in clinical outcomes with a reduction in the frequency and severity of maladaptive behaviors as defined in The Behavior Problem Inventory for Intellectual Disabilities Short Form.
Conclusion: Further investigation is required in comparing outcomes to other none integrated care models and work needs to be done to expand sample size. Despite limitations this early data is suggestive that integrated models of care should be considered in the IDD population, especially those with complex mental healthcare needs.
References:
Hughes-McCormack, L. A., Rydzewska, E., Henderson, A., MacIntyre, C., Rintoul, J., & Cooper, S. A. (2017). Prevalence of mental health conditions and relationship with general health in a whole-country population of people with intellectual disabilities compared with the general population. BJPsych open, 3(5), 243–248. https://doi.org/10.1192/bjpo.bp.117.005462
Reising V, Diegel-Vacek L, Dadabo Msw L, Corbridge S. Collaborative Care: Integrating Behavioral Health Into the Primary Care Setting. J Am Psychiatr Nurses Assoc. 2021 Aug 25:10783903211041653. doi: 10.1177/10783903211041653. Epub ahead of print. PMID: 34431726.
Background/Significance: The prevalence of mental illness among individuals with intellectual and developmental disabilities is greater than that of the general population. There is limited access to mental healthcare for adults with IDD in most communities. Patients often find themselves transitioning into the adult healthcare system with minimal support and few care options. The use of integrated care models can improve access to mental health care by building collaborative relationships between primary care providers, behavioral health specialists, and care management.
Methods: The University of Cincinnati Primary Care Network, The University of Cincinnati Department of Psychiatry, Cincinnati Children’s Hospital Medical Center, and Hamilton County Developmental Disabilities Services have partnered to form one such integrated care clinic. The focus is to identify individuals with complex psychosocial needs and to assist them in transitioning to adult care. In having an integrated care model where patients with IDD are able to obtain preventative medical care, acute medical care, psychiatric services, and support services there is expected to be overall improvement in patient/caregiver satisfaction and in clinical outcomes. Patient satisfaction scores was monitored via patient/caregiver surveys at the time of establishment in the integrated clinic, at six months, and at twelve months. Surveys were done looking at clinical outcomes. The Behavior Problem Inventory for Intellectual Disabilities Short Form was given at the same intervals to monitor changes in the frequently and severity of identified maladaptive behaviors.
Results: Following implementation of the integrated care model there was statistically significant improvement in patient satisfaction. Specifically there was improvement noted in the areas of care teams ability to meet unique needs, medical expertise of care team, and the collaboration between care team members. There was also statistically significant improvement in clinical outcomes with a reduction in the frequency and severity of maladaptive behaviors as defined in The Behavior Problem Inventory for Intellectual Disabilities Short Form.
Conclusion: Further investigation is required in comparing outcomes to other none integrated care models and work needs to be done to expand sample size. Despite limitations this early data is suggestive that integrated models of care should be considered in the IDD population, especially those with complex mental healthcare needs.
References:
Hughes-McCormack, L. A., Rydzewska, E., Henderson, A., MacIntyre, C., Rintoul, J., & Cooper, S. A. (2017). Prevalence of mental health conditions and relationship with general health in a whole-country population of people with intellectual disabilities compared with the general population. BJPsych open, 3(5), 243–248. https://doi.org/10.1192/bjpo.bp.117.005462
Reising V, Diegel-Vacek L, Dadabo Msw L, Corbridge S. Collaborative Care: Integrating Behavioral Health Into the Primary Care Setting. J Am Psychiatr Nurses Assoc. 2021 Aug 25:10783903211041653. doi: 10.1177/10783903211041653. Epub ahead of print. PMID: 34431726.
Corey Keeton, MD
Assistant Professor
University of Cincinnati
Cincinnati, Ohio, United States- LW
Lauren Wang, MD
Assistant Professor
University of Cincinnati
CINCINNATI, Ohio, United States