Back
Neurocognitive Disorders, Delirium and Neuropsychiatry
Poster Session
(104) Mania, Dressed and Undressed: A case of hepatic encephalopathy cloaking a diagnosis of bipolar disorder type 1
Abstract:
Background:
Presentations of mania in older individuals require special attention to organic etiologies. Two past case reports have associated hepatic encephalopathy with manic symptoms. Here we report a case of an individual with mania in the setting of recurrent hepatic encephalopathy who ultimately proved to have bipolar disorder.
Case:
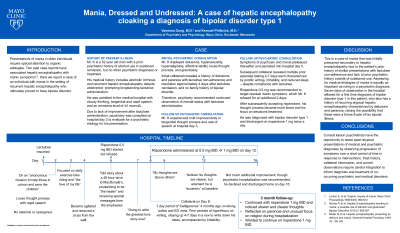
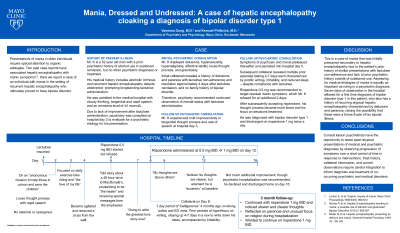
Mr. B is a 52 year old man with a prior psychiatric history of alcohol use in sustained remission, but no other psychiatric diagnoses or treatment. His medical history includes alcoholic cirrhosis and recurrent hepatic encephalopathy despite abstinence prompting longstanding lactulose administration. He was admitted to the medical hospital with cloudy thinking, tangential and rapid speech, and an ammonia level of 44 mcmol/L. Due to lack of improvement after lactulose administration, psychiatry was consulted on hospital day 2 to evaluate for a psychiatric etiology for his presentation. Mr. B was noted to display delusions, hypersexuality, hyperreligiosity, affective lability, loose thought process, and grandiosity. Initial collateral revealed a history of delusions and paranoia with lactulose non-adherence and resolution approximately 4 days after lactulose reinitiation, and no family history of bipolar disorder. Therefore, psychiatry recommended continued observation of mental status with lactulose administration. He experienced mild improvements in tangential thought process and rate of speech at hospital day 3. However, symptoms of psychosis and mania plateaued thereafter and persisted into hospital day 5. Subsequent collateral revealed past periods of 4-5 days of hyperfocus on writing, irritability, and reduced sleep. Risperidone 0.5 mg was recommended to target residual manic and psychotic symptoms, which Mr. B refused for an additional 2 days. After subsequently accepting risperidone, his thought process became more linear and his focus on delusions lessened. He was diagnosed with bipolar disorder type 1 and discharged on risperidone 1 mg twice a day.
Discussion:
This is a case of mania that was initially presumed secondary to hepatic encephalopathy due to the patient’s prior history of similar presentations with lactulose non-adherence and lack of prior psychiatric history outside of substance use. Assessing for medical etiologies of mania is equally as important as ruling in a psychiatric diagnosis. Seven days of observation in the hospital allowed for a first time diagnosis of bipolar disorder type 1 in this patient, who also has a history of recurring atypical hepatic encephalopathy characterized by delusions and paranoia, raising the possibility that these were a forme fruste of his bipolar illness. Conclusions/implications:
Consult liaison psychiatrists have the opportunity to tease apart atypical presentations of medical and psychiatric diagnoses by observing progression of symptoms over a short period of time in response to interventions. Past history, collateral information, and current observations require careful integration to inform diagnosis and treatment of co-occurring psychiatric and medical disorders.
Background:
Presentations of mania in older individuals require special attention to organic etiologies. Two past case reports have associated hepatic encephalopathy with manic symptoms. Here we report a case of an individual with mania in the setting of recurrent hepatic encephalopathy who ultimately proved to have bipolar disorder.
Case:
Mr. B is a 52 year old man with a prior psychiatric history of alcohol use in sustained remission, but no other psychiatric diagnoses or treatment. His medical history includes alcoholic cirrhosis and recurrent hepatic encephalopathy despite abstinence prompting longstanding lactulose administration. He was admitted to the medical hospital with cloudy thinking, tangential and rapid speech, and an ammonia level of 44 mcmol/L. Due to lack of improvement after lactulose administration, psychiatry was consulted on hospital day 2 to evaluate for a psychiatric etiology for his presentation. Mr. B was noted to display delusions, hypersexuality, hyperreligiosity, affective lability, loose thought process, and grandiosity. Initial collateral revealed a history of delusions and paranoia with lactulose non-adherence and resolution approximately 4 days after lactulose reinitiation, and no family history of bipolar disorder. Therefore, psychiatry recommended continued observation of mental status with lactulose administration. He experienced mild improvements in tangential thought process and rate of speech at hospital day 3. However, symptoms of psychosis and mania plateaued thereafter and persisted into hospital day 5. Subsequent collateral revealed past periods of 4-5 days of hyperfocus on writing, irritability, and reduced sleep. Risperidone 0.5 mg was recommended to target residual manic and psychotic symptoms, which Mr. B refused for an additional 2 days. After subsequently accepting risperidone, his thought process became more linear and his focus on delusions lessened. He was diagnosed with bipolar disorder type 1 and discharged on risperidone 1 mg twice a day.
Discussion:
This is a case of mania that was initially presumed secondary to hepatic encephalopathy due to the patient’s prior history of similar presentations with lactulose non-adherence and lack of prior psychiatric history outside of substance use. Assessing for medical etiologies of mania is equally as important as ruling in a psychiatric diagnosis. Seven days of observation in the hospital allowed for a first time diagnosis of bipolar disorder type 1 in this patient, who also has a history of recurring atypical hepatic encephalopathy characterized by delusions and paranoia, raising the possibility that these were a forme fruste of his bipolar illness. Conclusions/implications:
Consult liaison psychiatrists have the opportunity to tease apart atypical presentations of medical and psychiatric diagnoses by observing progression of symptoms over a short period of time in response to interventions. Past history, collateral information, and current observations require careful integration to inform diagnosis and treatment of co-occurring psychiatric and medical disorders.

Vanessa Dang, MD (she/her/hers)
Psychiatry Resident
Mayo Clinic
Rochester, MN, United States- KP
Kemuel Philbrick, MD
Consultant
Mayo Clinic
Rochester, Minnesota, United States