Back
Quality and Safety
Poster Session
(148) Patient Perspectives on No-Shows in Behavioral Health Settings
Abstract:
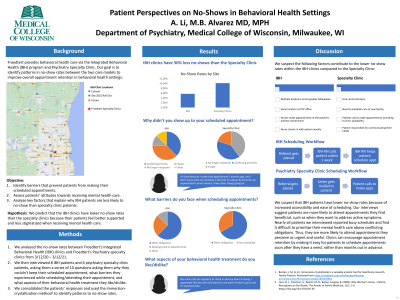
Background: Patients who “no-show” their appointments by failing to keep their scheduled times negatively impact the clinic’s workflow and productivity2, which is why it’s important to address common reasons patients miss appointments. We found that no-show rates for mental health appointments within Froedtert’s Integrated Behavioral Health (IBH) clinics is about 50% of Froedtert’s Psychiatry specialty clinics, so we interviewed patients from each clinic to identify key factors that may explain this discrepancy.
Methods: We interviewed 8 IBH patients and 6 psychiatry specialty clinic patients who missed their behavioral health appointments from 9/1/21-11/30/21. We asked each patient a series of 10 questions, asking them why they couldn’t keep their scheduled appointment, what barriers they experienced while scheduling/attending their appointment, and what aspects of their behavioral health treatment they like/dislike. After conducting the interviews, we consolidated the patients’ responses and used the immersion-crystallization method1 to identify patterns contributing towards no-shows.
Results: The main reason IBH and specialty clinic patients could not keep their scheduled appointments is because a conflicting priority came up, or they forgot about their appointment. 1 IBH patient and 2 specialty clinic patients reported that they didn’t feel a strong urge to make their appointment because they didn’t have an active issue and didn’t think seeing going to the doctor was important anymore. The main barrier both IBH and specialty clinic patients experienced when scheduling/attending their appointments was other obligations such as work, school, kids, etc. When asked what aspects of their behavioral health treatment they liked/disliked, the majority of patients in both groups reported working with their care team. The IBH patients reported greater satisfaction in ease of scheduling than the specialty clinic patients, noting that it was fairly easy to get an appointment that fit their schedule.
Discussion: We suspect that IBH patients have lower no-show rates because of increased accessibility and ease of scheduling. Our interviews suggest patients are more likely to attend appointments they find beneficial, such as when they want to address active symptoms. Furthermore, nearly all the patients we interviewed have busy schedules and find it difficult to prioritize their mental health care above conflicting obligations. Thus, they are more likely to attend appointments they perceive as urgent and useful.
Conclusion: We can reduce no-show rates in behavioral health settings by changing the scheduling system so patients can quickly make an appointment when they have a medical concern.
References:
< !1. < Borkan, J. M. (n.d.). Immersion–Crystallization: a valuable analytic tool for healthcare research. Family Practice. Retrieved from https://academic.oup.com/fampra/advance-article/doi/10.1093/fampra/cmab158/6439963 >
< 2. < Lacy, N. L., Paulman, A., Reuter, M. D., & Lovejoy, B. (2003). Why We Don't Come – Patient Perceptions on No-Shows. The Annals of Family Medicine, 1(1), 2–4. https://doi.org/10.1370/afm.46 >
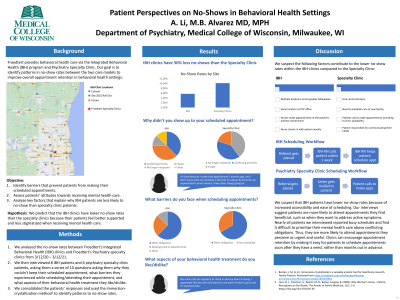
Background: Patients who “no-show” their appointments by failing to keep their scheduled times negatively impact the clinic’s workflow and productivity2, which is why it’s important to address common reasons patients miss appointments. We found that no-show rates for mental health appointments within Froedtert’s Integrated Behavioral Health (IBH) clinics is about 50% of Froedtert’s Psychiatry specialty clinics, so we interviewed patients from each clinic to identify key factors that may explain this discrepancy.
Methods: We interviewed 8 IBH patients and 6 psychiatry specialty clinic patients who missed their behavioral health appointments from 9/1/21-11/30/21. We asked each patient a series of 10 questions, asking them why they couldn’t keep their scheduled appointment, what barriers they experienced while scheduling/attending their appointment, and what aspects of their behavioral health treatment they like/dislike. After conducting the interviews, we consolidated the patients’ responses and used the immersion-crystallization method1 to identify patterns contributing towards no-shows.
Results: The main reason IBH and specialty clinic patients could not keep their scheduled appointments is because a conflicting priority came up, or they forgot about their appointment. 1 IBH patient and 2 specialty clinic patients reported that they didn’t feel a strong urge to make their appointment because they didn’t have an active issue and didn’t think seeing going to the doctor was important anymore. The main barrier both IBH and specialty clinic patients experienced when scheduling/attending their appointments was other obligations such as work, school, kids, etc. When asked what aspects of their behavioral health treatment they liked/disliked, the majority of patients in both groups reported working with their care team. The IBH patients reported greater satisfaction in ease of scheduling than the specialty clinic patients, noting that it was fairly easy to get an appointment that fit their schedule.
Discussion: We suspect that IBH patients have lower no-show rates because of increased accessibility and ease of scheduling. Our interviews suggest patients are more likely to attend appointments they find beneficial, such as when they want to address active symptoms. Furthermore, nearly all the patients we interviewed have busy schedules and find it difficult to prioritize their mental health care above conflicting obligations. Thus, they are more likely to attend appointments they perceive as urgent and useful.
Conclusion: We can reduce no-show rates in behavioral health settings by changing the scheduling system so patients can quickly make an appointment when they have a medical concern.
References:
< !1. < Borkan, J. M. (n.d.). Immersion–Crystallization: a valuable analytic tool for healthcare research. Family Practice. Retrieved from https://academic.oup.com/fampra/advance-article/doi/10.1093/fampra/cmab158/6439963 >
< 2. < Lacy, N. L., Paulman, A., Reuter, M. D., & Lovejoy, B. (2003). Why We Don't Come – Patient Perceptions on No-Shows. The Annals of Family Medicine, 1(1), 2–4. https://doi.org/10.1370/afm.46 >

Anji Li (she/her/hers)
Medical Student
Medical College of Wisconsin
Wauwatosa, WI, United States
Mary Beth Alvarez, MD, MPH
Assistant Professor
Medical College of Wisconsin
Fox Point, Wisconsin, United States