Back
Poster, Podium & Video Sessions
Moderated Poster
MP08: Pediatric Urology: Penis & Scrotum
MP08-01: Operative Outcomes of Pediatric Non-Congenital Urethroplasty at a Single Tertiary Care Institution
Friday, May 13, 2022
10:30 AM – 11:45 AM
Location: Room 225
James Ding*, Sameer Mittal, Jason Van Batavia, Dana Weiss, Stephen Zderic, Mark Zaontz, Aseem Shukla, Arun Srinivasan, Christopher Long, Robert Kovell, Philadelphia, PA

James Morgan Ding, MD (he/him/his)
Resident
University of Pennsylvania
Poster Presenter(s)
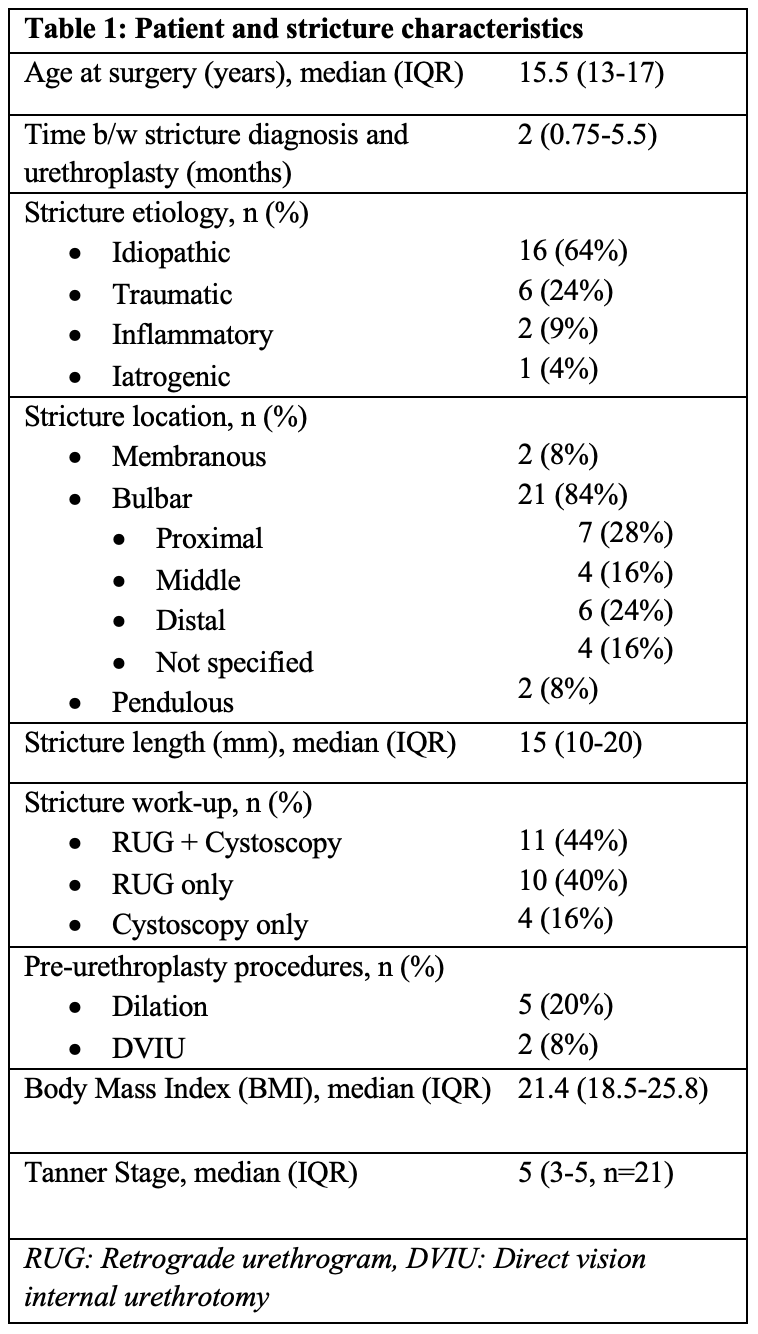
Introduction: The dearth of studies regarding pediatric non-congenitally related urethroplasty leaves much information to be extrapolated from the adult population. The aim of this study is to evaluate outcomes for pediatric, non-congenital urethroplasty at a tertiary care center.
Methods: The EMR was queried for male pediatric ( <18 y/o) patients who underwent urethroplasty (excluding those related to congenital disease) at one tertiary care institution between 2012-2020. Procedure success was defined as a) post-op uroflow improvement or RUG showing resolution of stricture, b) resolution of presenting symptoms, and c) no additional procedures performed.
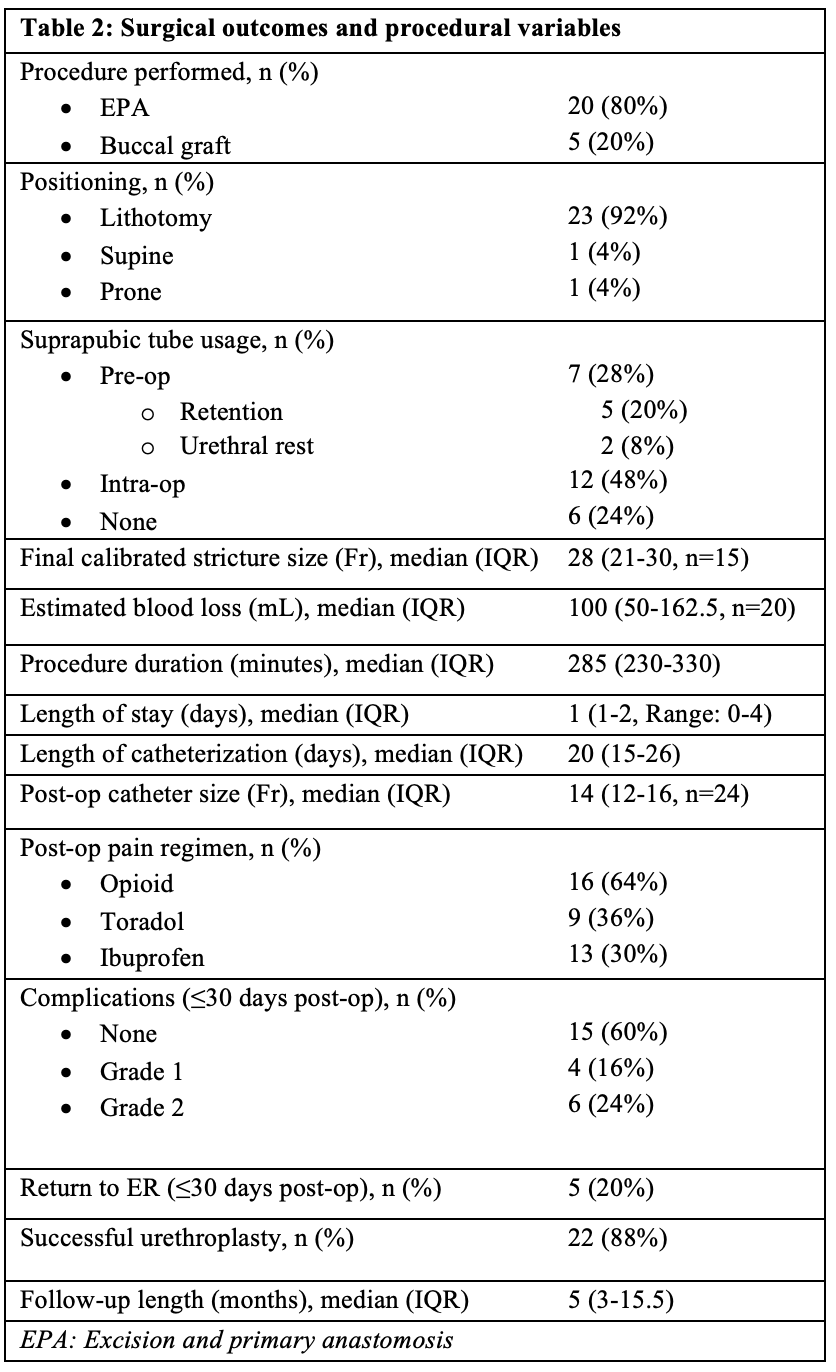
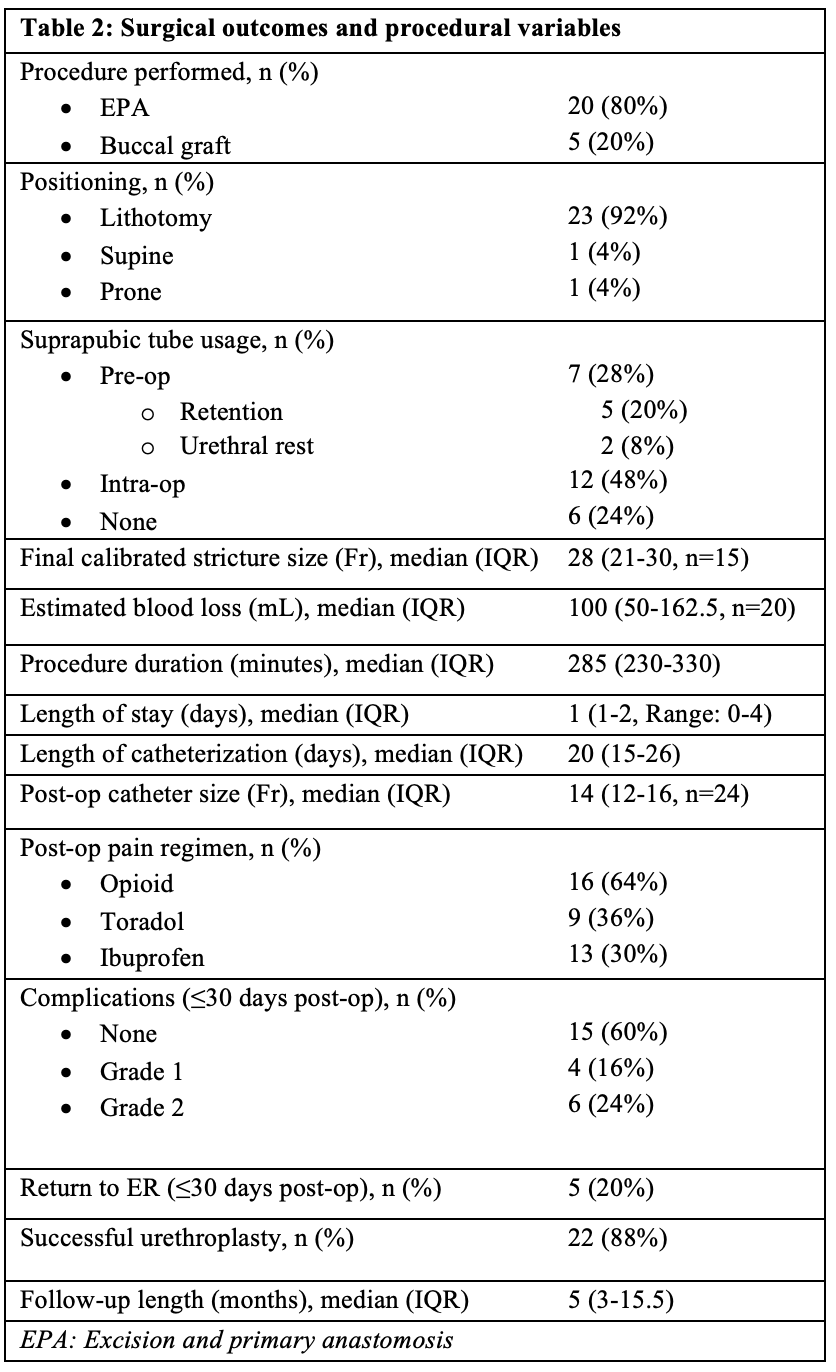
Results: 25 pediatric patients underwent non-congenital urethroplasty during the study period (median age at surgery, 15.5 years). The majority of strictures had idiopathic etiology (64%) and were bulbar in location (84%). 7 (28%) patients underwent either dilation or DVIU prior to urethroplasty. 20 (80%) underwent EPA and 4 (20%) were treated with buccal grafting. One buccal graft underwent a staged procedure, with a tunica vaginalis flap used for the 2nd stage.
22 (88%) of patients had a successful urethroplasty as previously defined. Median follow-up length was 5 months (IQR: 3-15.5). Of the non-successes, two had stricture recurrence (at 2- and 6-years post-op) requiring DVIU and repeat urethroplasty, respectively, while one had ongoing lower urinary tract symptoms despite a normal post-operative urethral caliber.
Conclusions: This single-institution series supports the idea that non-congenitally related pediatric urethroplasties, while rare, are safely done and highly successful. Recurrence of strictures years out from initial surgeries demonstrate the importance of following this group long-term, particularly when defining surgical “success” with symptomatic/multi-factor criteria. Incorporating patient reported outcome measures, such as sexual function, is a promising area of future study, particularly for an adolescent population.
Source of Funding: N/A
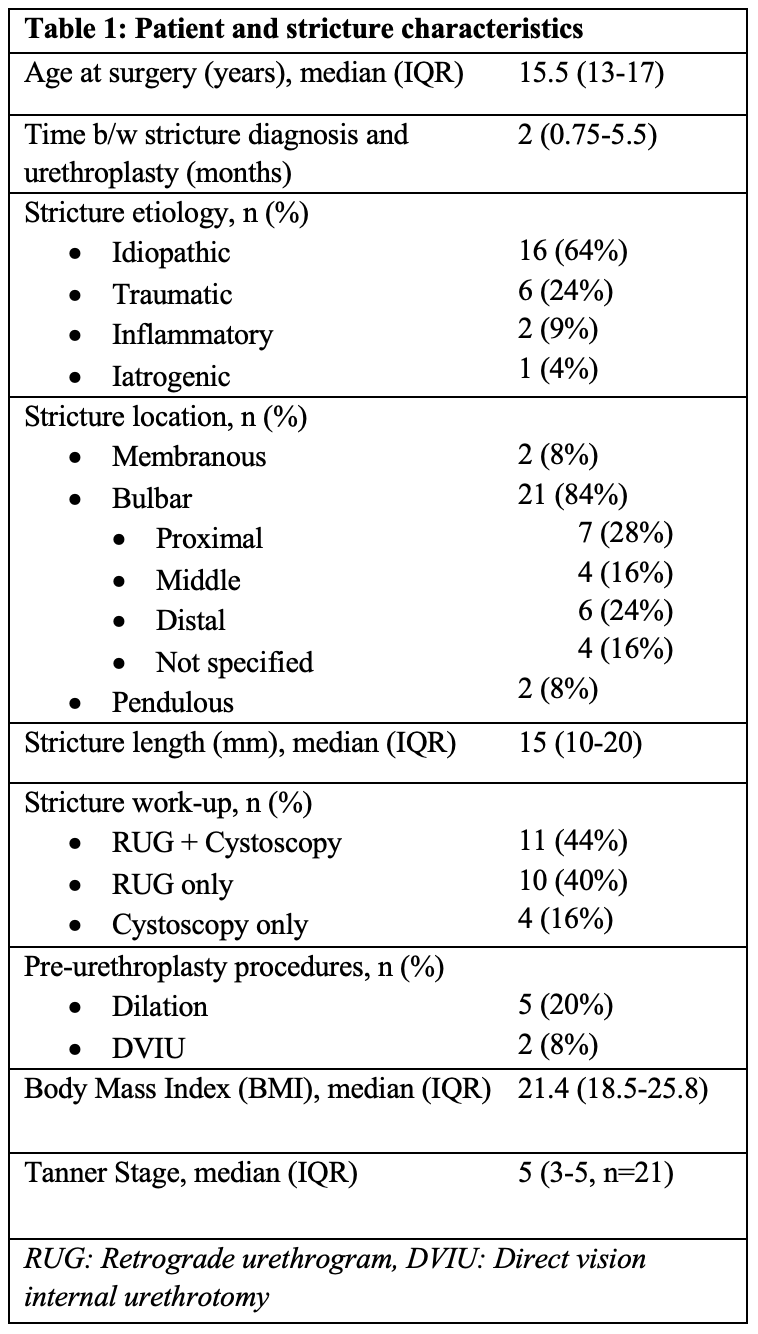
Methods: The EMR was queried for male pediatric ( <18 y/o) patients who underwent urethroplasty (excluding those related to congenital disease) at one tertiary care institution between 2012-2020. Procedure success was defined as a) post-op uroflow improvement or RUG showing resolution of stricture, b) resolution of presenting symptoms, and c) no additional procedures performed.
Results: 25 pediatric patients underwent non-congenital urethroplasty during the study period (median age at surgery, 15.5 years). The majority of strictures had idiopathic etiology (64%) and were bulbar in location (84%). 7 (28%) patients underwent either dilation or DVIU prior to urethroplasty. 20 (80%) underwent EPA and 4 (20%) were treated with buccal grafting. One buccal graft underwent a staged procedure, with a tunica vaginalis flap used for the 2nd stage.
22 (88%) of patients had a successful urethroplasty as previously defined. Median follow-up length was 5 months (IQR: 3-15.5). Of the non-successes, two had stricture recurrence (at 2- and 6-years post-op) requiring DVIU and repeat urethroplasty, respectively, while one had ongoing lower urinary tract symptoms despite a normal post-operative urethral caliber.
Conclusions: This single-institution series supports the idea that non-congenitally related pediatric urethroplasties, while rare, are safely done and highly successful. Recurrence of strictures years out from initial surgeries demonstrate the importance of following this group long-term, particularly when defining surgical “success” with symptomatic/multi-factor criteria. Incorporating patient reported outcome measures, such as sexual function, is a promising area of future study, particularly for an adolescent population.
Source of Funding: N/A

.jpg)
.jpg)