Back
Poster, Podium & Video Sessions
Moderated Poster
MP10: Education Research I
MP10-10: Head-to-head Comparison of Hydrogel Models to Cadavers for Inflatable Penile Prosthesis (IPP) Training
Friday, May 13, 2022
1:00 PM – 2:15 PM
Location: Room 228
Patrick Saba*, Rachel Melnyk, Michael Witthaus, Christopher Wanderling, Tyler Holler, Ahmed Ghazi, Rochester, NY
.jpg)
Patrick Saba, BA,MS
SUNY Upstate Medical University
Poster Presenter(s)
Introduction: Cadavers have long been the standard for inflatable penile prosthetic (IPP) placement training. However limited availability, biohazard risk and specialized facilities hinders their widespread use. A previously validated high-fidelity, non-biohazardous, hydrogel procedural model for IPP placement was developed to address this need. We aim to evaluate if hydrogel models can adequately perform as an equivalent training tool for IPP placement to supplement standard cadaveric simulations.
Methods: 73 participants (12 experts, 13 fellows, 48 residents) performed guided IPP simulations on a cadaver followed by a hydrogel model (Figure 1). Surveys were completed to compare tissue properties, anatomical and procedural resemblance, and educational effectiveness between the two modalities on a 5-point Likert scale.
Results: 86% of participants agreed the hydrogel training model replicated relevant human anatomy. 86% agreed that the hydrogel tissues resembled the appearance of cadaveric tissues with participants also agreeing the dartos (92%), scrotum (90%), pubic bone (88%), skin (86%), and corpora (71%) resembled the texture/behavior of a cadaver. 96%, 94%, 93%, 89%, 89%, 86% agreed that the model replicated procedural steps in cadavers, regarding prosthesis measurement and placement, stay suture placement, tissue closure, corporal dilation, and skin/dartos incision respectively.
100% of experts and fellows agreed the model is useful for: improving technical skills, teaching the procedure, and assessing procedural ability vs 94%, 96%, and 88% of residents respectively. 75% of experts believed that the hydrogel model was equal if not better than cadavers at these respective categories. 83% of participants agreed the model was safer than cadavers and 75% agreed the model was equal if not better than cadavers as an educational tool. 82% (75%, 92%, 81% of experts, fellows, residents, respectively) stated they wish to include the models alongside current cadaver training with 1/4 of experts stating they preferred the models over cadavers.
Conclusions: This procedural simulation allows the practice of each step of IPP placement with equivalent fidelity to standard cadaveric simulations. Its non-biohazardous nature provides a safe and effective educational equivalent for IPP surgical training.
Source of Funding: Coloplast Research Grant
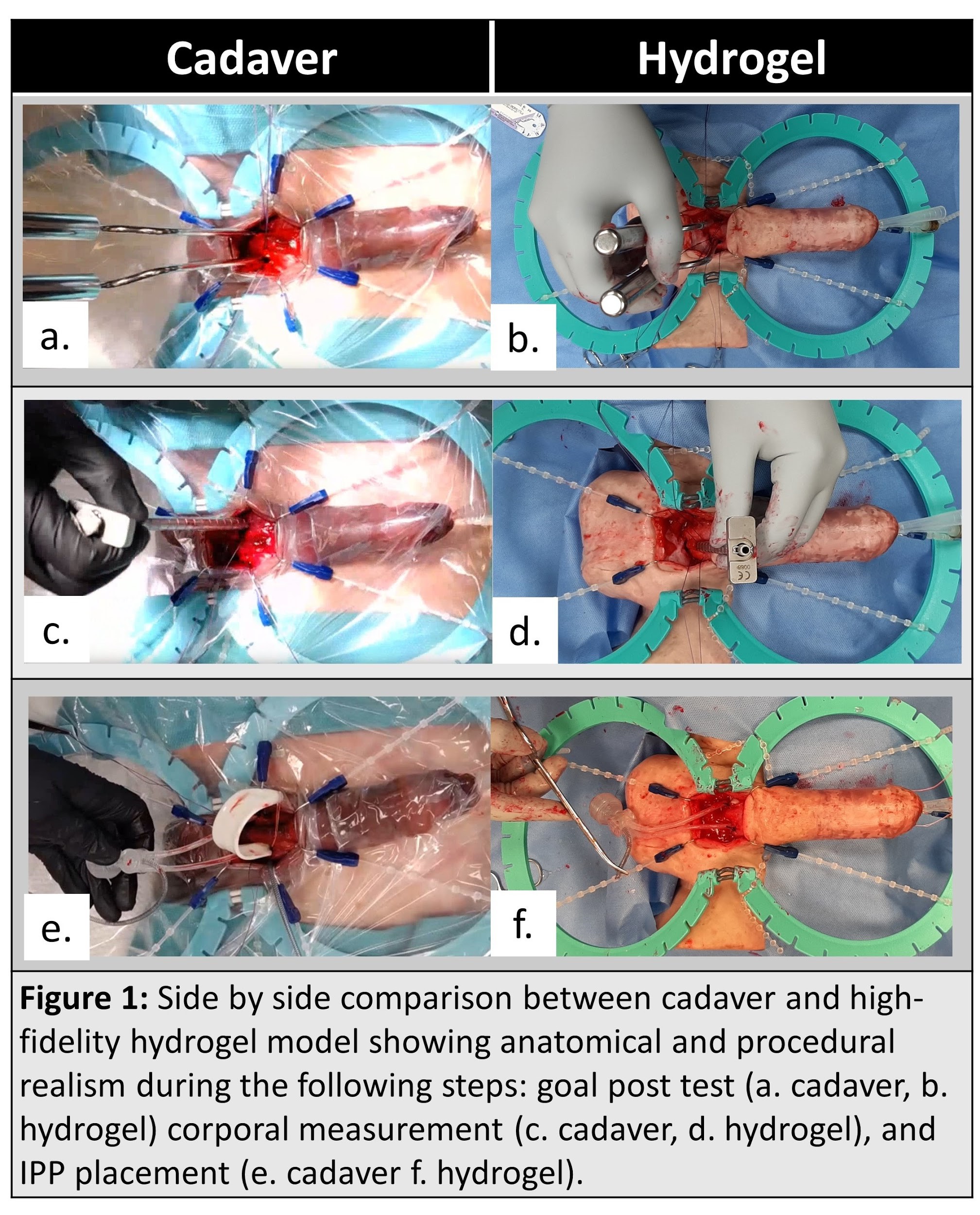
Methods: 73 participants (12 experts, 13 fellows, 48 residents) performed guided IPP simulations on a cadaver followed by a hydrogel model (Figure 1). Surveys were completed to compare tissue properties, anatomical and procedural resemblance, and educational effectiveness between the two modalities on a 5-point Likert scale.
Results: 86% of participants agreed the hydrogel training model replicated relevant human anatomy. 86% agreed that the hydrogel tissues resembled the appearance of cadaveric tissues with participants also agreeing the dartos (92%), scrotum (90%), pubic bone (88%), skin (86%), and corpora (71%) resembled the texture/behavior of a cadaver. 96%, 94%, 93%, 89%, 89%, 86% agreed that the model replicated procedural steps in cadavers, regarding prosthesis measurement and placement, stay suture placement, tissue closure, corporal dilation, and skin/dartos incision respectively.
100% of experts and fellows agreed the model is useful for: improving technical skills, teaching the procedure, and assessing procedural ability vs 94%, 96%, and 88% of residents respectively. 75% of experts believed that the hydrogel model was equal if not better than cadavers at these respective categories. 83% of participants agreed the model was safer than cadavers and 75% agreed the model was equal if not better than cadavers as an educational tool. 82% (75%, 92%, 81% of experts, fellows, residents, respectively) stated they wish to include the models alongside current cadaver training with 1/4 of experts stating they preferred the models over cadavers.
Conclusions: This procedural simulation allows the practice of each step of IPP placement with equivalent fidelity to standard cadaveric simulations. Its non-biohazardous nature provides a safe and effective educational equivalent for IPP surgical training.
Source of Funding: Coloplast Research Grant

.jpg)
.jpg)