Back
Poster, Podium & Video Sessions
Moderated Poster
MP13: Health Services Research: Practice Patterns, Quality of Life and Shared Decision Making I
MP13-05: Urologist Hiring Practices: Data from the American Urological Association 2020 Census
Friday, May 13, 2022
2:45 PM – 4:00 PM
Location: Room 228
Christina Shin*, Justin Loloi, Bronx, NY, Raymond Fang, Linthicum, MD, William Meeks, Maryland, MD, Andrew Harris, Lexington, KY, Amanda North, Bronx, NY

Christina Shin, BA
Albert Einstein College of Medicine
Poster Presenter(s)
Introduction: Multiple estimates suggest an impending shortage of urologists secondary to an aging urology workforce, leading to more urologists exiting rather than entering practice. We sought to better understand factors concerning urologist recruitment, hiring, and perceived barriers to professional success in order to identify areas to support future urologists.
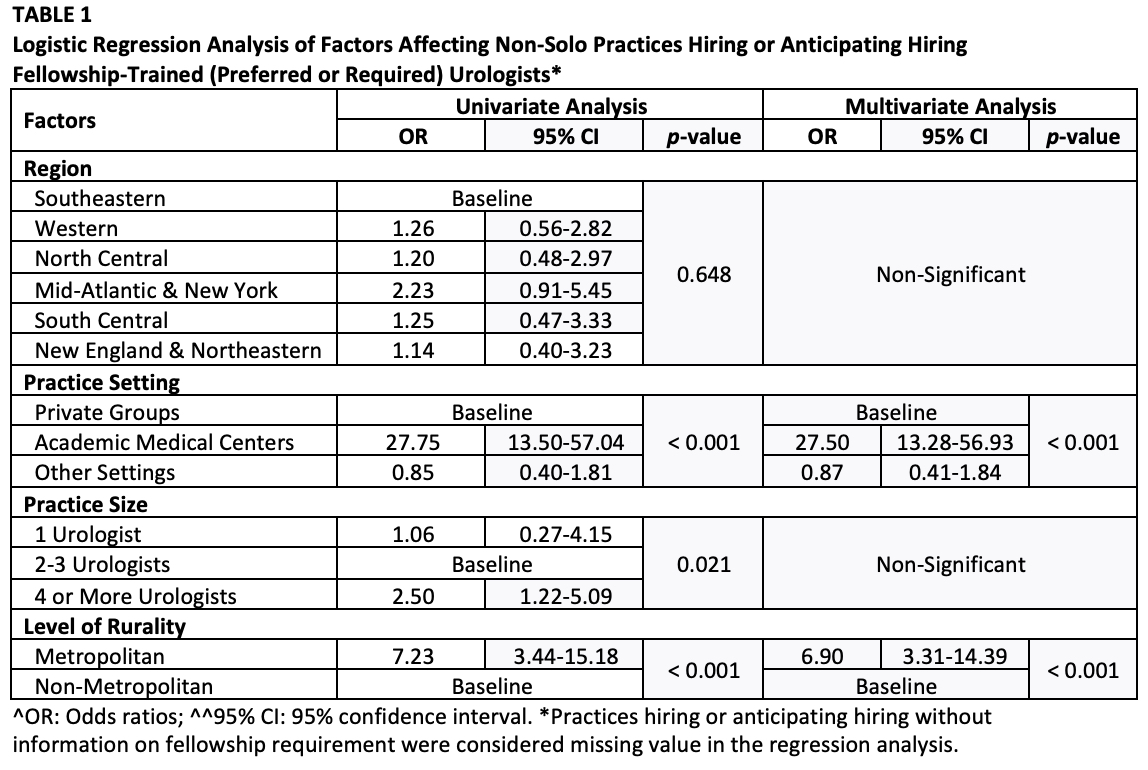
Methods: We analyzed survey data from the 2020 American Urological Association (AUA) Annual Census regarding urologist recruitment patterns, compensation, use of resources, and professional barriers. Multivariate logistic regression was used to analyze hiring patterns, while adjusting for practice region, setting, size, and level of rurality.
Results: Of 13,352 practicing urologists in 2020, 1,972 (14.8%) completed the Census. 23.3% of urologic practices reported hiring or were anticipating hiring, with higher rates in the South Central (35.7%) and New England and Northeastern (35.2%) region and lower rates in the North Central (28.6%) region. Academic medical centers (93.3%) were more likely to hire compared to private group practices (33.3%) (OR: 1.66 [95% CI: 1.02-2.72]) on multivariate analysis.
A majority of private groups (66.7%) did not prefer or require fellowship in recruitment, suggesting the relative lack of need of specialty training for resident-graduates entering the non-academic setting. Conversely, academic medical centers sought fellowship trained providers (93.3%). Academic medical centers (OR: 27.5 [95% CI: 13.28-56.93]) and the urology practices in metropolitan areas (OR: 6.90 [95% CI: 3.31-14.39]) were more likely to hire fellowship trained urologists on multivariate analysis (Table 1).
More female urologists (93%) reported barriers to professional success compared to their male counterparts (74.5%). The most cited barrier for females was lack of control over staffing decisions or scheduling (46.2%), whereas the most cited barrier for males was lack of time (33.7%).
Conclusions: These findings illustrate variability in hiring practicing and barriers to success. With a better understanding of these issues, we can offer targeted avenues of support for future urologists, including guidance in negotiating contracts and alleviating barriers to professional success.
Source of Funding: None
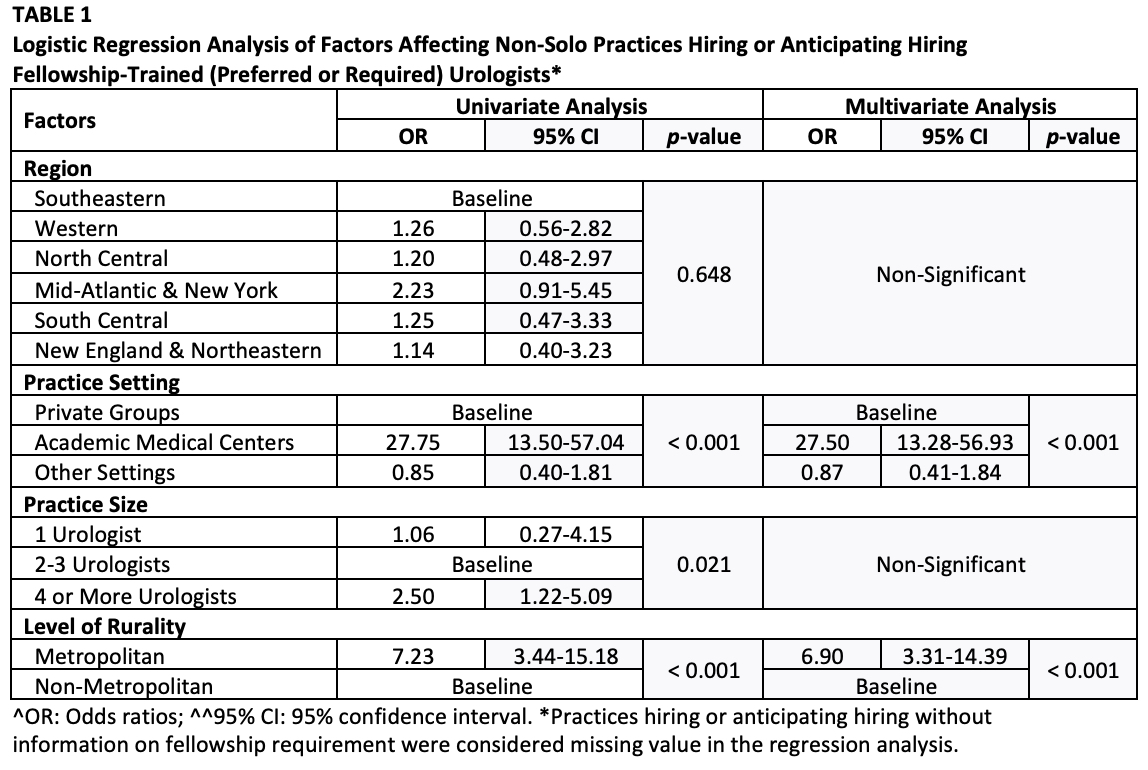
Methods: We analyzed survey data from the 2020 American Urological Association (AUA) Annual Census regarding urologist recruitment patterns, compensation, use of resources, and professional barriers. Multivariate logistic regression was used to analyze hiring patterns, while adjusting for practice region, setting, size, and level of rurality.
Results: Of 13,352 practicing urologists in 2020, 1,972 (14.8%) completed the Census. 23.3% of urologic practices reported hiring or were anticipating hiring, with higher rates in the South Central (35.7%) and New England and Northeastern (35.2%) region and lower rates in the North Central (28.6%) region. Academic medical centers (93.3%) were more likely to hire compared to private group practices (33.3%) (OR: 1.66 [95% CI: 1.02-2.72]) on multivariate analysis.
A majority of private groups (66.7%) did not prefer or require fellowship in recruitment, suggesting the relative lack of need of specialty training for resident-graduates entering the non-academic setting. Conversely, academic medical centers sought fellowship trained providers (93.3%). Academic medical centers (OR: 27.5 [95% CI: 13.28-56.93]) and the urology practices in metropolitan areas (OR: 6.90 [95% CI: 3.31-14.39]) were more likely to hire fellowship trained urologists on multivariate analysis (Table 1).
More female urologists (93%) reported barriers to professional success compared to their male counterparts (74.5%). The most cited barrier for females was lack of control over staffing decisions or scheduling (46.2%), whereas the most cited barrier for males was lack of time (33.7%).
Conclusions: These findings illustrate variability in hiring practicing and barriers to success. With a better understanding of these issues, we can offer targeted avenues of support for future urologists, including guidance in negotiating contracts and alleviating barriers to professional success.
Source of Funding: None

.jpg)
.jpg)