Back
Poster, Podium & Video Sessions
Moderated Poster
MP19: Education Research II
MP19-06: Prospective evaluation of postoperative pain and opioid use after minor urologic surgery
Saturday, May 14, 2022
7:00 AM – 8:15 AM
Location: Room 228
Bonnie Liu*, Kevin Feng, Jeffrey Campbell, London, Canada

Bonnie Liu, MD
University of Western Ontario
Poster Presenter(s)
Introduction: Filling an opioid prescription after a minor urologic procedure increases patient risk of overdose and misuse. Strategies to reduce the number of opioids reaching the community are critical. This study evaluates the opioid utilization after minor urologic procedures at a Canadian academic center and guide future prescribing recommendations.
Methods: We prospectively evaluated patients over 18 years old undergoing minor urologic procedures (penile, scrotal, urethral, etc.) from September 2020 to October 2021. Consenting participants were given a pain diary and post-operative pain questionnaire. Patients on chronic pain medications or had major surgery within 6 months were excluded. Response rate, pain on visual analog scale, pain control satisfaction, quantity of opioids prescribed, and consumption of opioid and non-opioid medication were collected and analyzed.
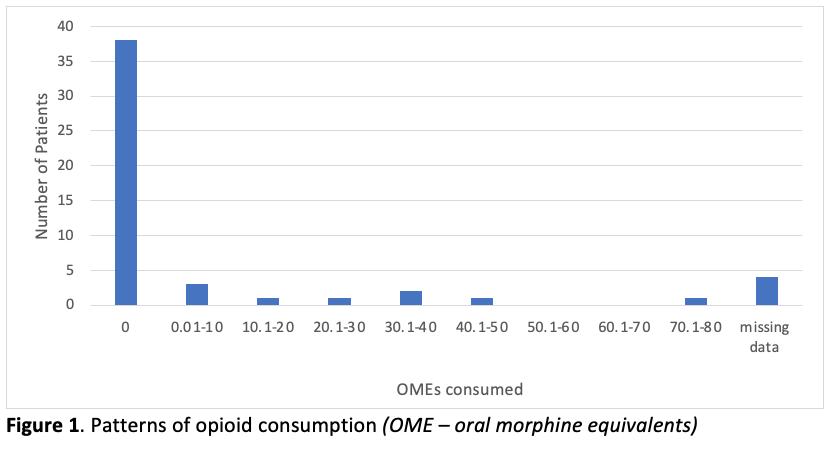
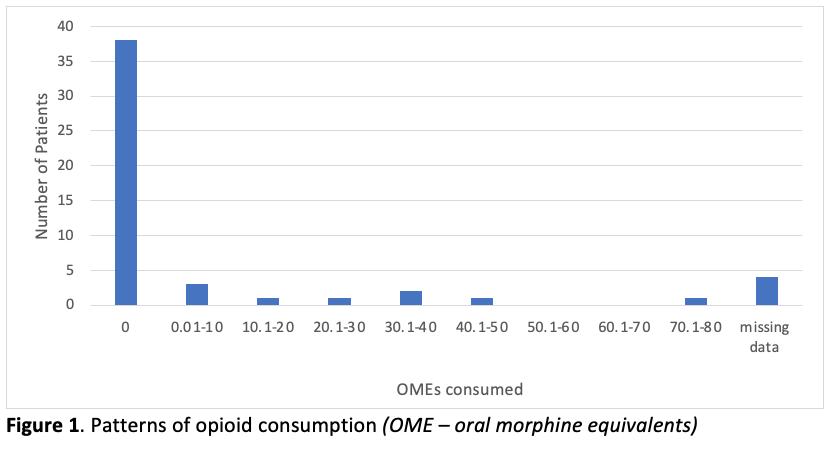
Results: Eighty-four patients met the inclusion criteria. The mean age was 61.3 years (range:20-87 years) and 97% of patients identify as male. The response rate for the opioid diary and pain questionnaire was 61%. Thirty-nine patients (76%) were offered an opioid prescription following their surgery, but only thirteen of those patients (33%) filled and consumed any opioids analgesics. Forty patients (78%) used no post-operative opioids, and the mean oral morphine equivalents (OME) consumed was 5 (standard deviation 14.6). There were 89 unused opioid tablets from post-procedure prescriptions. The mean overall pain score for patients who did and did not fill opioid prescriptions were 3.5/10 and 1.8/10 (p=0.053), respectively, with mean overall pain management satisfaction score of 8.2/10 and 8.8/10 (p=0.432), respectively.
Conclusions: Most patients undergoing minor urologic procedures do not require opioids to manage post-operative pain. Based on our data, we suggest that a prescription for 35 OMEs would adequately treat post-operative pain in 95% of patients undergoing minor urologic procedures. Education around pain management with non-narcotic modalities is imperative, and practice changes are warranted to address the opioid crisis within our specialty.
Source of Funding: Department of Surgery, University of Western Ontario, Internal research fund
Methods: We prospectively evaluated patients over 18 years old undergoing minor urologic procedures (penile, scrotal, urethral, etc.) from September 2020 to October 2021. Consenting participants were given a pain diary and post-operative pain questionnaire. Patients on chronic pain medications or had major surgery within 6 months were excluded. Response rate, pain on visual analog scale, pain control satisfaction, quantity of opioids prescribed, and consumption of opioid and non-opioid medication were collected and analyzed.
Results: Eighty-four patients met the inclusion criteria. The mean age was 61.3 years (range:20-87 years) and 97% of patients identify as male. The response rate for the opioid diary and pain questionnaire was 61%. Thirty-nine patients (76%) were offered an opioid prescription following their surgery, but only thirteen of those patients (33%) filled and consumed any opioids analgesics. Forty patients (78%) used no post-operative opioids, and the mean oral morphine equivalents (OME) consumed was 5 (standard deviation 14.6). There were 89 unused opioid tablets from post-procedure prescriptions. The mean overall pain score for patients who did and did not fill opioid prescriptions were 3.5/10 and 1.8/10 (p=0.053), respectively, with mean overall pain management satisfaction score of 8.2/10 and 8.8/10 (p=0.432), respectively.
Conclusions: Most patients undergoing minor urologic procedures do not require opioids to manage post-operative pain. Based on our data, we suggest that a prescription for 35 OMEs would adequately treat post-operative pain in 95% of patients undergoing minor urologic procedures. Education around pain management with non-narcotic modalities is imperative, and practice changes are warranted to address the opioid crisis within our specialty.
Source of Funding: Department of Surgery, University of Western Ontario, Internal research fund

.jpg)
.jpg)