Back
Poster, Podium & Video Sessions
Moderated Poster
MP20: Trauma/Reconstruction/Diversion: External Genitalia Reconstruction and Urotrauma (including transgender surgery) I
MP20-07: Urology consultation is associated with adherence to imaging guidelines and decreased nephrectomy in high grade renal trauma
Saturday, May 14, 2022
7:00 AM – 8:15 AM
Location: Room 225
Shirley Wang, Pranjal Agrawal*, Mary Rostom, Nikita Gupta, Albert Holler, Isabelle Pan, Kent Stevens, Raymond Fang, Elliott Haut, Ryan Fransman, Renu Berry, Andrew Cohen, Baltimore, MD
.jpg)
Pranjal Agrawal, BA
Johns Hopkins School of Medicine
Poster Presenter(s)
Introduction: Renal trauma is unique in that acute management involves the trauma team, primarily urology, or joint management. The ideal management pathway has yet to be established. We aim to describe rates of urology consultation following renal trauma and assess subsequent impact on imaging and intervention.
Methods: We conducted an IRB-approved retrospective review of patients at a Level I trauma center sustaining renal trauma between 2014 and 2021. Demographic, injury, radiologic, and intervention variables were extracted and compared by urology and trauma surgery management using chi-squared, Fischer’s exact tests, and Mann-Whitney U tests. All available images were ultimately graded using American Association for the Surgery of Trauma (AAST) scoring. Analyses were performed using STATA with p<0.05 considered significant.
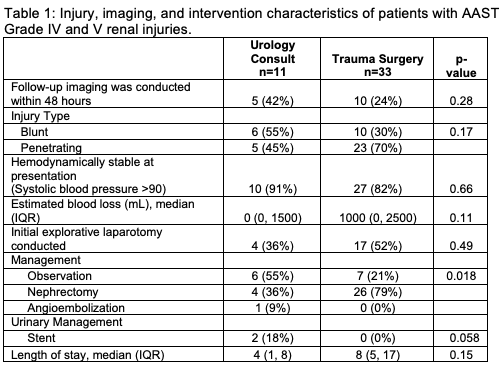
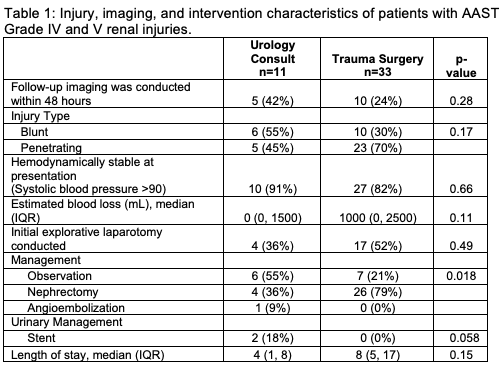
Results: From 2014-2021, 118 patients with median age 29 (IQR 22-41) incurred renal trauma. Urology was consulted in 18 (15.3%) cases. Demographic and injury characteristics were similar between the two groups. AAST renal injury grade was transcribed in the initial radiologic reports for 49 (41.5%) of patients. Among the full cohort including AAST grade I through V injuries, urology consult was associated with greater likelihood of receiving delayed contrast imaging (50.0% vs. 17.0%, p=0.002); however, there was no significant difference in rate of follow-up imaging within 48 hours among patients with grade IV and V injuries (Table 1). In this sub-group, there was no significant difference in rates of penetrating injury or whether an initial exploratory laparotomy was conducted. Of patients with high-grade injuries, those with urology consult were less likely to undergo nephrectomy (36% vs. 79%, p=0.018).
Conclusions: We observed differences in imaging patterns between renal trauma patients who are managed primarily by trauma surgery versus urology. However, the further downstream impact of these differences in imaging remains to be elucidated. Among patients with high-grade renal trauma, urology consult was associated with decreased rate of nephrectomy, highlighting the feasibility of renal salvage in a multidisciplinary trauma setting. In our center, future quality improvement may involve improved compliance with AAST Renal Trauma Grading.
Source of Funding: N/A
Methods: We conducted an IRB-approved retrospective review of patients at a Level I trauma center sustaining renal trauma between 2014 and 2021. Demographic, injury, radiologic, and intervention variables were extracted and compared by urology and trauma surgery management using chi-squared, Fischer’s exact tests, and Mann-Whitney U tests. All available images were ultimately graded using American Association for the Surgery of Trauma (AAST) scoring. Analyses were performed using STATA with p<0.05 considered significant.
Results: From 2014-2021, 118 patients with median age 29 (IQR 22-41) incurred renal trauma. Urology was consulted in 18 (15.3%) cases. Demographic and injury characteristics were similar between the two groups. AAST renal injury grade was transcribed in the initial radiologic reports for 49 (41.5%) of patients. Among the full cohort including AAST grade I through V injuries, urology consult was associated with greater likelihood of receiving delayed contrast imaging (50.0% vs. 17.0%, p=0.002); however, there was no significant difference in rate of follow-up imaging within 48 hours among patients with grade IV and V injuries (Table 1). In this sub-group, there was no significant difference in rates of penetrating injury or whether an initial exploratory laparotomy was conducted. Of patients with high-grade injuries, those with urology consult were less likely to undergo nephrectomy (36% vs. 79%, p=0.018).
Conclusions: We observed differences in imaging patterns between renal trauma patients who are managed primarily by trauma surgery versus urology. However, the further downstream impact of these differences in imaging remains to be elucidated. Among patients with high-grade renal trauma, urology consult was associated with decreased rate of nephrectomy, highlighting the feasibility of renal salvage in a multidisciplinary trauma setting. In our center, future quality improvement may involve improved compliance with AAST Renal Trauma Grading.
Source of Funding: N/A

.jpg)
.jpg)