Back
Poster, Podium & Video Sessions
Moderated Poster
MP20: Trauma/Reconstruction/Diversion: External Genitalia Reconstruction and Urotrauma (including transgender surgery) I
MP20-12: Assessment of Neophallus Length Following Metoidioplasty
Saturday, May 14, 2022
7:00 AM – 8:15 AM
Location: Room 225
Hannah Glick*, Stephanie Diagnault-Newton, Miriam Hadj-Moussa, Ann Arbor, MI

Hannah Glick, BS
University of Michigan
Poster Presenter(s)
Introduction: An increasing number of transgender and gender diverse individuals are presenting to care for gender affirming services. Genital gender affirming surgery (gGAS) improves quality of life and sexual satisfaction. An option for gGAS in transmasculine individuals is the metoidioplasty, creating a small neophallus from enlarged clitoral tissue following prolonged testosterone exposure. A commonly asked question for patients considering metoidioplasty is what size neophallus they can expect postoperatively. There are currently no studies to date which have shown how preoperative stretched clitoral length correlates with postoperative exposed neophallus length. The goal of this study is to understand factors which contribute to greater exposed neophallus length following metoidioplasty.
Methods: We performed a retrospective chart review on patients from 2000-2021 presenting to a single academic institution who underwent a metoidioplasty utilizing the Belgrade style technique, with or without urethral lengthening.
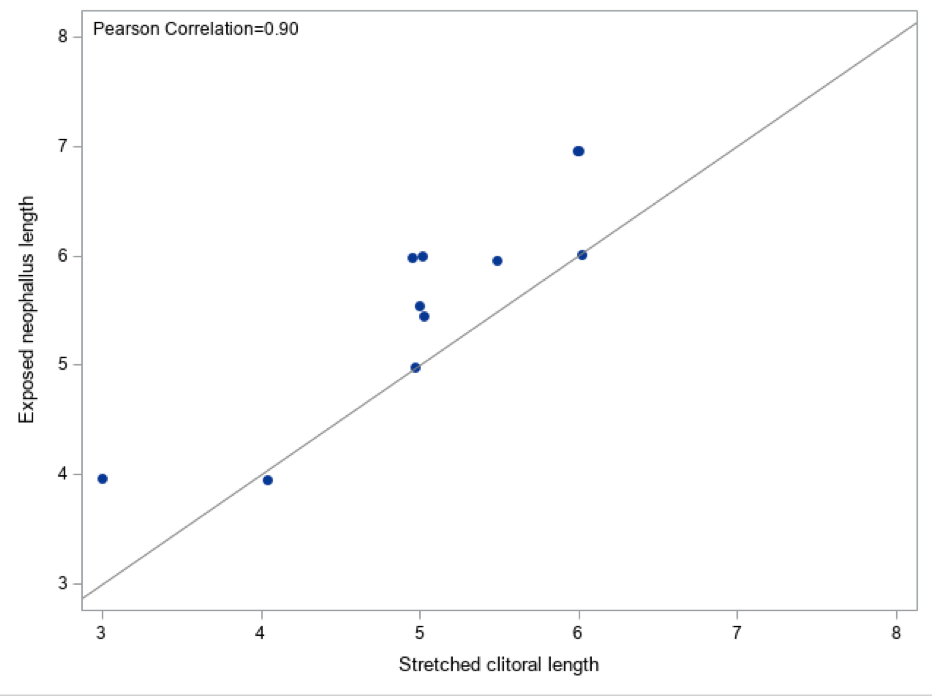
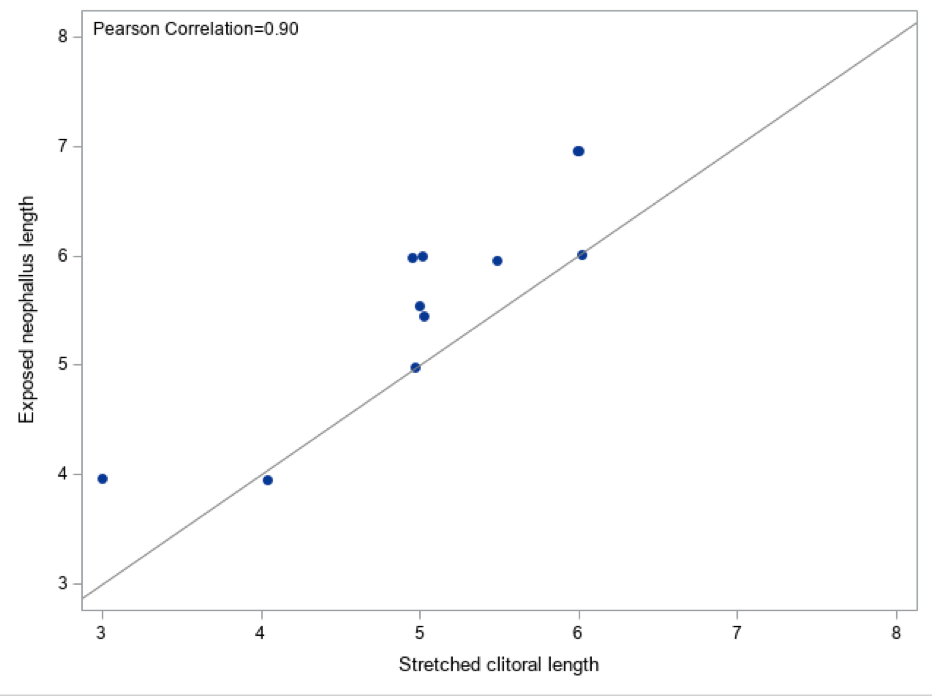
Results: A total of 23 patients underwent metoidioplasty. Of those patients, 11 had recorded stretched clitoral length (preoperatively) and exposed neophallus length (postoperatively). There were 9 (82%) patients who identified as transgender men, and 2 (18%) who identified as nonbinary. In this cohort, the median length on testosterone was 4.1 years. The median stretched clitoral length was 5cm, the median exposed neophallus length was 6cm. There was a strong correlation between preoperative length and postoperative length (?=0.9) (figure 1). Increased length on testosterone was not associated with longer exposed neophallus length (p=0.09) and had a negative correlation (?=-0.53).
Conclusions: Patients considering metoidioplasty understandably wonder how large their neophallus will be after surgery. We’ve found that patients can expect postoperative neophallus exposed length to be about 1cm larger than their preoperative stretched clitoral length. A longer time on testosterone is not associated with longer exposed neophallus length. Our study was limited by its small sample size. Future studies should be done to elucidate factors which may preclude to longer exposed neophallus length after metoidioplasty. This information is crucial for our gender diverse patients to make informed decisions about gGAS.
Source of Funding: None
Methods: We performed a retrospective chart review on patients from 2000-2021 presenting to a single academic institution who underwent a metoidioplasty utilizing the Belgrade style technique, with or without urethral lengthening.
Results: A total of 23 patients underwent metoidioplasty. Of those patients, 11 had recorded stretched clitoral length (preoperatively) and exposed neophallus length (postoperatively). There were 9 (82%) patients who identified as transgender men, and 2 (18%) who identified as nonbinary. In this cohort, the median length on testosterone was 4.1 years. The median stretched clitoral length was 5cm, the median exposed neophallus length was 6cm. There was a strong correlation between preoperative length and postoperative length (?=0.9) (figure 1). Increased length on testosterone was not associated with longer exposed neophallus length (p=0.09) and had a negative correlation (?=-0.53).
Conclusions: Patients considering metoidioplasty understandably wonder how large their neophallus will be after surgery. We’ve found that patients can expect postoperative neophallus exposed length to be about 1cm larger than their preoperative stretched clitoral length. A longer time on testosterone is not associated with longer exposed neophallus length. Our study was limited by its small sample size. Future studies should be done to elucidate factors which may preclude to longer exposed neophallus length after metoidioplasty. This information is crucial for our gender diverse patients to make informed decisions about gGAS.
Source of Funding: None

.jpg)
.jpg)