Back
Poster, Podium & Video Sessions
Moderated Poster
MP24: Kidney Cancer: Localized: Surgical Therapy I
MP24-10: Impact of hemostatic agents on surgical complications and hospital costs in patients undergoing partial nephrectomy in the United States
Saturday, May 14, 2022
8:45 AM – 10:00 AM
Location: Room 222
Kendrick Yim*, Jose I Nolaazco, Yuzhe Tang, Marie-Therese Valovska, Kevin R Melnick, Logan Briggs, Boston, MA, Benjamin I Chung, Stanford, CA, Steven L Chang, Boston, MA
- KY
Poster Presenter(s)
Introduction: To examine the cost and effect of hemostatic agents (HA) on surgical and perioperative outcomes in patients undergoing partial nephrectomy.
Methods: We performed a retrospective cohort study of adult patients undergoing elective partial nephrectomy (PN) from January 2016 to December 2017 at 416 US hospitals using the Premier Hospital Database by surgeons performing at least 10 cases annually. We reviewed Chargemaster data to determine the median cost of commonly used HA, and performed multivariable quantile regression analysis to assess the impact of hemostatic agents on 90-day direct hospital costs for PN. To assess the clinical impact of HA and to minimize unmeasured biases, a subgroup multivariable logistic regression analysis was performed comparing patients from surgeons always using HA versus surgeons never using HA with respect to 90-day complications (Clavien-Dindo and bleeding) and readmission, operating room time, and length of stay.
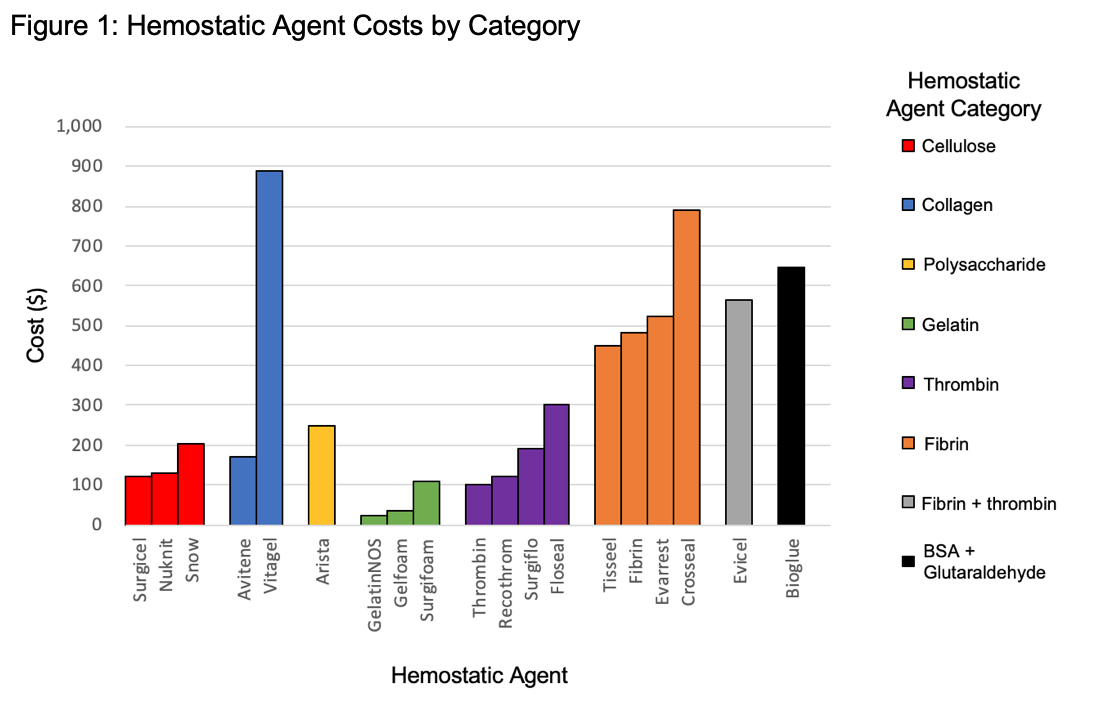
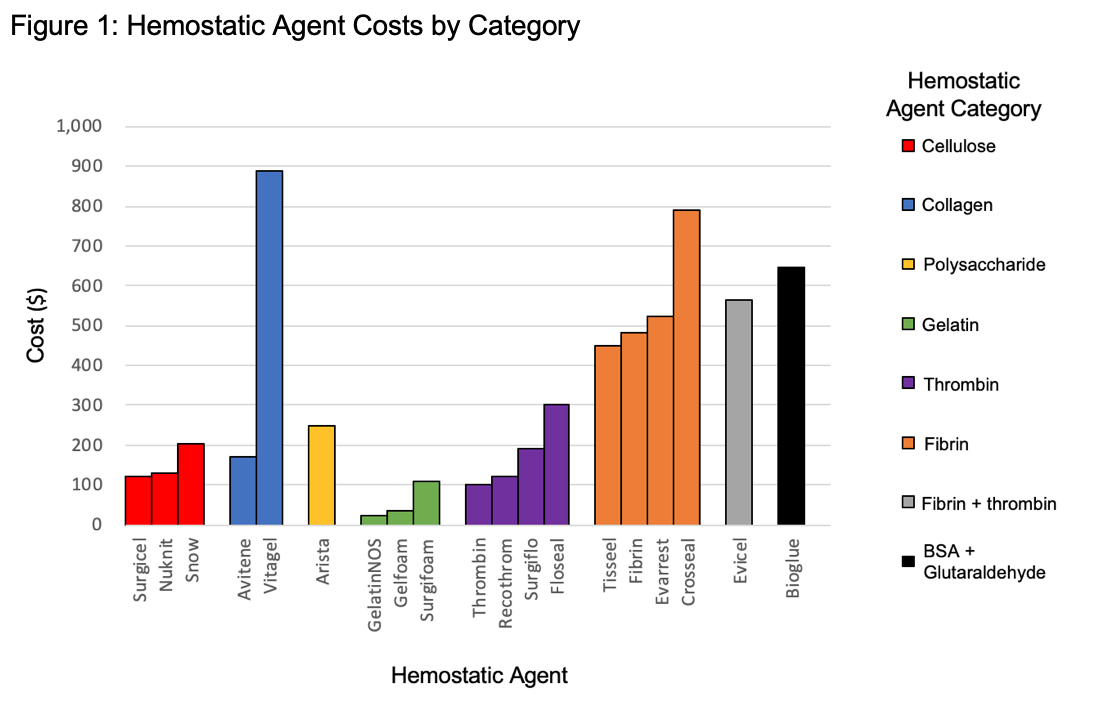
Results: A total of 9380 patients were included in the study (median age: 61 years, male: 59.8%) with 7603 (81.1%) receiving HA and 1777 (18.9%) not receiving HA during surgery. Chargemaster data revealed that the median cost of HA ranged from US$34 to US$888 per application (Figure 1). Use of HA increased PN costs by $1358 (95% CI, $965 – $1750). In the subgroup analysis, comparing 556 patients with surgeons always using HA to 4328 patients never using HA, there was no difference in complications (OR 0.91; 95% CI 0.7 – 1.17), bleeding (OR 0.83; 95% CI 0.59 – 1.17), operating room time (+1 min; 95% CI -11 min – 12 min), length of stay (OR 0.95, 95%CI 0.69 – 1.31), or readmission (OR 1.39, 95%CI 0.74 – 2.62).
Conclusions: Utilization of HA is common for patients undergoing PN. While HA use increases the cost of surgery, it does not appear to uniformly benefit surgical complications, readmission, length of stay, bleeding, or operating room time. While HA clearly play an important role in minimizing surgical hemorrhage, surgeons should utilize these agents judiciously on a case-by-case basis in order to maximize benefit and minimize system-wide cost. More research is needed to understand the specific situations and which HA are most appropriate for PN.
Source of Funding: None
Methods: We performed a retrospective cohort study of adult patients undergoing elective partial nephrectomy (PN) from January 2016 to December 2017 at 416 US hospitals using the Premier Hospital Database by surgeons performing at least 10 cases annually. We reviewed Chargemaster data to determine the median cost of commonly used HA, and performed multivariable quantile regression analysis to assess the impact of hemostatic agents on 90-day direct hospital costs for PN. To assess the clinical impact of HA and to minimize unmeasured biases, a subgroup multivariable logistic regression analysis was performed comparing patients from surgeons always using HA versus surgeons never using HA with respect to 90-day complications (Clavien-Dindo and bleeding) and readmission, operating room time, and length of stay.
Results: A total of 9380 patients were included in the study (median age: 61 years, male: 59.8%) with 7603 (81.1%) receiving HA and 1777 (18.9%) not receiving HA during surgery. Chargemaster data revealed that the median cost of HA ranged from US$34 to US$888 per application (Figure 1). Use of HA increased PN costs by $1358 (95% CI, $965 – $1750). In the subgroup analysis, comparing 556 patients with surgeons always using HA to 4328 patients never using HA, there was no difference in complications (OR 0.91; 95% CI 0.7 – 1.17), bleeding (OR 0.83; 95% CI 0.59 – 1.17), operating room time (+1 min; 95% CI -11 min – 12 min), length of stay (OR 0.95, 95%CI 0.69 – 1.31), or readmission (OR 1.39, 95%CI 0.74 – 2.62).
Conclusions: Utilization of HA is common for patients undergoing PN. While HA use increases the cost of surgery, it does not appear to uniformly benefit surgical complications, readmission, length of stay, bleeding, or operating room time. While HA clearly play an important role in minimizing surgical hemorrhage, surgeons should utilize these agents judiciously on a case-by-case basis in order to maximize benefit and minimize system-wide cost. More research is needed to understand the specific situations and which HA are most appropriate for PN.
Source of Funding: None

.jpg)
.jpg)