Back
Poster, Podium & Video Sessions
Moderated Poster
MP25: Trauma/Reconstruction/Diversion: Ureter (including Pyeloplasty) and Bladder Reconstruction (including fistula), Augmentation, Substitution, Diversion
MP25-09: Multi-Institutional Comparison of Non-Transecting Versus Transecting Primary Robotic Pyeloplasty for Ureteropelvic Junction Obstruction: The Collaborative of Reconstructive Robotic Ureteral Surgery (CORRUS) Experience
Saturday, May 14, 2022
10:30 AM – 11:45 AM
Location: Room 228
David Strauss*, Matthew Lee, Philadelphia, PA, Ziho Lee, Chicago, IL, Aeen Asghar, Randall Lee, Philadelphia, PA, Lee Zhao, New York, NY, Michael Stifelman, Hackensack, NJ, Daniel Eun, Philadelphia, PA
- DS
David M. Strauss, MD
Lewis Katz School of Medicine at Temple University Hospital
Poster Presenter(s)
Introduction: There is a paucity of literature describing non-transecting pyeloplasty in the primary setting of ureteropelvic junction obstruction (UPJO) repair. Our objective is to describe the surgical techniques and peri-operative outcomes of primary non-transecting robotic pyeloplasty (RP) compared to standard dismembered RP.
Methods: The Collaborative of Reconstructive Robotic Ureteral Surgery (CORRUS) multi-institutional database was queried retrospectively for all patients who underwent primary RP between 04/2012-08/2020. Patients were grouped according to surgical approach; Anderson-Hynes dismembered (transecting) RP or non-transecting RP (Fenger or Y-V Flap). Perioperative outcomes were compared using nonparametric independent sample median tests and chi-square tests; p<0.05 was considered significant.
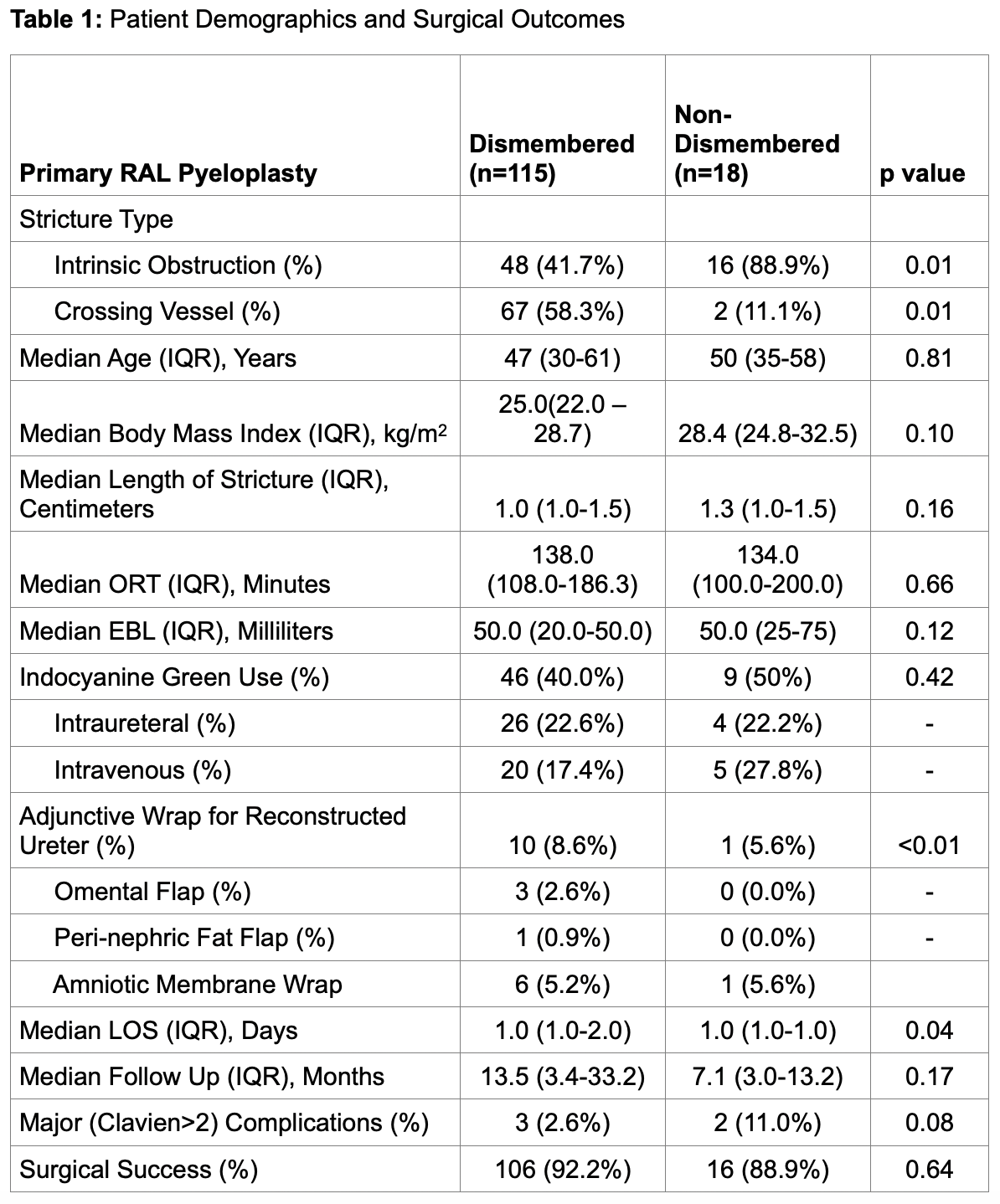
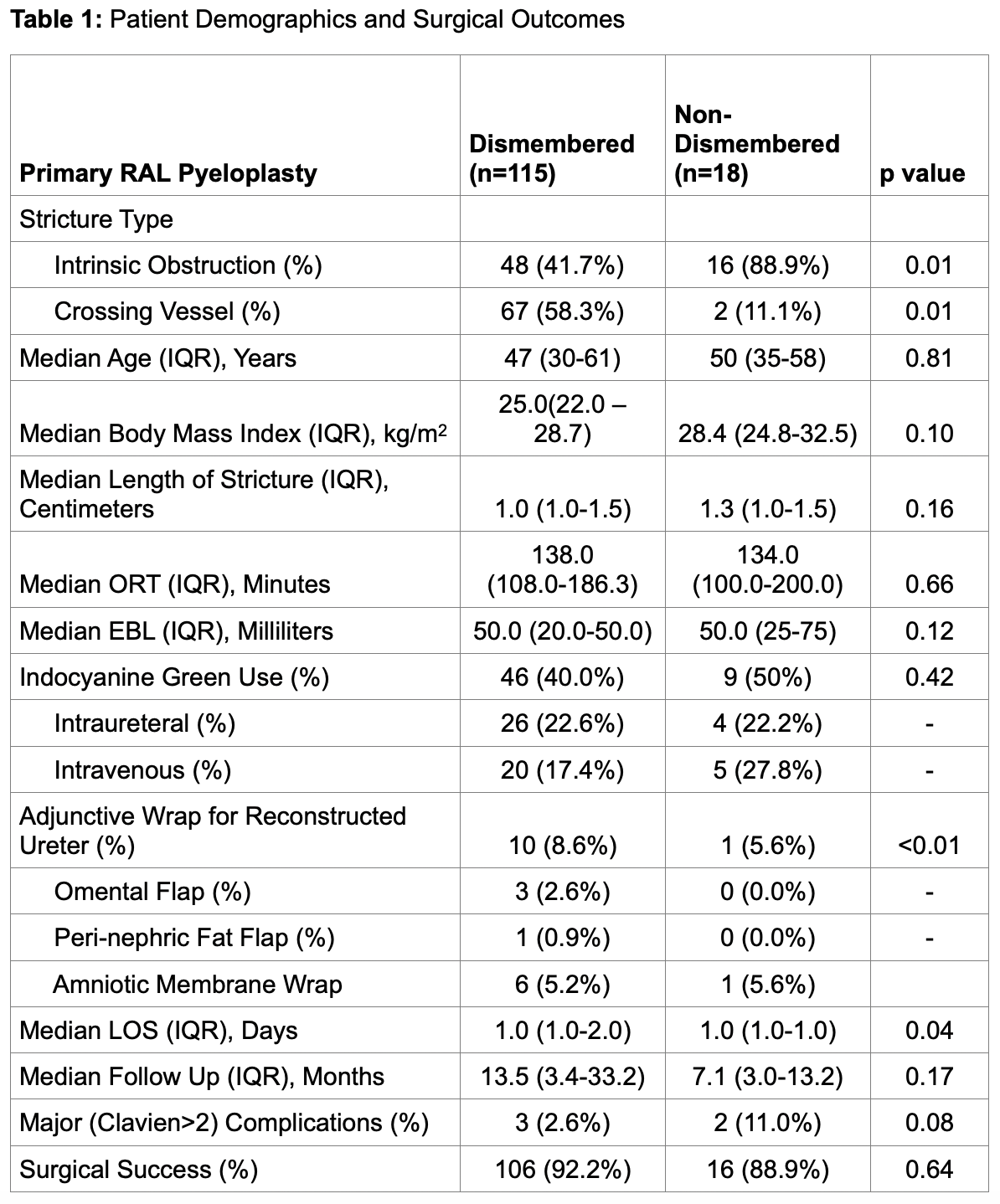
Results: Of 133 patients, 115 (86.5%) underwent transecting and 18 (13.5%) underwent non-transecting RP. Median operative time (138.0 vs 134.0 min, p=0.66) and estimated blood loss (50 vs 50cc, p=0.12) were similar between transecting and non-transecting groups, respectively. Likewise, there was no difference in major (Clavien>2) complications between the surgical technique groups (p=0.08). At a median follow-up of 12.9 months, there was no difference in success between transecting and non transecting groups (92.2% versus 88.9%, respectively; p=0.64).
Conclusions: Given variable anatomical configurations of ureteropelvic junction obstruction (UPJO), including ureteral, vascular, and perihilar variations, a “one-size-fits-all” approach to pyeloplasty is inappropriate. Primary non-transecting RP, compared to standard dismembered RP, showed similar operative time, EBL, complication rates, as well as surgical success. The authors do not intend to suggest non transecting pyeloplasty replace dismembered pyeloplasty in the primary setting, especially for indications such as a crossing vessel; however rather hope to demonstrate that a primary non transecting approach in select patients is not inferior to a dismembered approach, and serves as an important technique in the armamentarium of the robotic urologist approaching difficult UPJO repairs.
Source of Funding: N/A
Methods: The Collaborative of Reconstructive Robotic Ureteral Surgery (CORRUS) multi-institutional database was queried retrospectively for all patients who underwent primary RP between 04/2012-08/2020. Patients were grouped according to surgical approach; Anderson-Hynes dismembered (transecting) RP or non-transecting RP (Fenger or Y-V Flap). Perioperative outcomes were compared using nonparametric independent sample median tests and chi-square tests; p<0.05 was considered significant.
Results: Of 133 patients, 115 (86.5%) underwent transecting and 18 (13.5%) underwent non-transecting RP. Median operative time (138.0 vs 134.0 min, p=0.66) and estimated blood loss (50 vs 50cc, p=0.12) were similar between transecting and non-transecting groups, respectively. Likewise, there was no difference in major (Clavien>2) complications between the surgical technique groups (p=0.08). At a median follow-up of 12.9 months, there was no difference in success between transecting and non transecting groups (92.2% versus 88.9%, respectively; p=0.64).
Conclusions: Given variable anatomical configurations of ureteropelvic junction obstruction (UPJO), including ureteral, vascular, and perihilar variations, a “one-size-fits-all” approach to pyeloplasty is inappropriate. Primary non-transecting RP, compared to standard dismembered RP, showed similar operative time, EBL, complication rates, as well as surgical success. The authors do not intend to suggest non transecting pyeloplasty replace dismembered pyeloplasty in the primary setting, especially for indications such as a crossing vessel; however rather hope to demonstrate that a primary non transecting approach in select patients is not inferior to a dismembered approach, and serves as an important technique in the armamentarium of the robotic urologist approaching difficult UPJO repairs.
Source of Funding: N/A

.jpg)
.jpg)