Back
Poster, Podium & Video Sessions
Moderated Poster
MP39: Health Services Research: Value of Care: Cost and Outcomes Measures
MP39-05: Urology Advanced Practice Providers in Rural America: An Opportunity to Provide Care
Sunday, May 15, 2022
8:45 AM – 10:00 AM
Location: Room 228
Jennifer Nauheim*, Bronx, NY, Raymond Fang, William Meeks, Keonna Confesor, Linthicum, MD, Amanda North, Bronx, NY
Jennifer Nauheim, MD
Montefiore Medical Center
Poster Presenter(s)
Introduction: There is a shortage of urologists in rural counties with up to 62% having no urologist at all in 2020. Advanced Practice Providers (APPs) including Physician Assistants (PAs) and Nurse Practitioners (NPs) could supplement this shortage to provide necessary urologic care where needed.
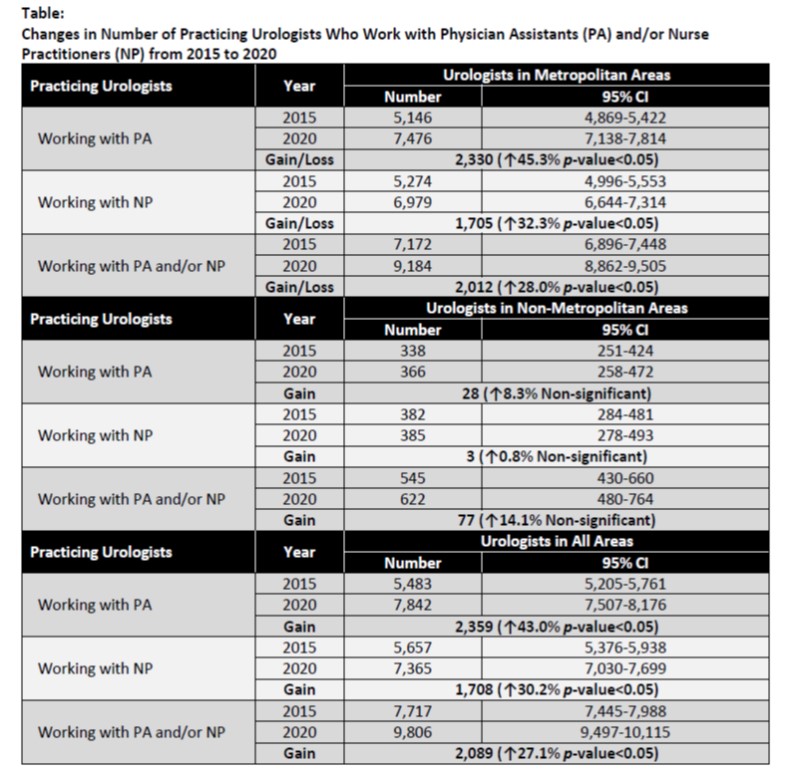
Methods: The American Urological Association (AUA) annual census data was used to compare APP growth rates from 2015 to 2020 in metropolitan and non-metropolitan areas in the United States. An area with a population size of 50,000 or more was defined as a metropolitan area. In contrast, an area with a population size under 50,000 was defined as a non-metropolitan area. Counts and growth rates of PAs and NPs or collectively APPs were calculated between 2015 and 2020.
Results: The number of practicing urologists who worked with physician assistants (PA) and nurse practitioners (NP) increased from 5,146 and 5,272 in 2015 to 7,476 and 6,979 in 2020. The growth rates of urologists who worked with PA and NP were much higher in metropolitan areas (45.3% and 32.3% or overall 28.0%) compared to non-metropolitan areas (8.3% and 0.8% or overall 14.1%) from 2015 to 2020.
Conclusions: There is a known shortage of urologists in rural counties and urologists who practice in rural areas are less likely to have APPs on staff. APPs are known to benefit urologic practices by reducing patient waiting times, improving overall productivity, and improving patient education. APPs may also serve a benefit in providing urologic care where there is no urologist. The number of practicing urologists working with APPs has increased over the past five years however there is a significant difference in the growth rate of urologists working with APPs in metropolitan areas than in non-metropolitan areas. The slower growth of urologists who worked with APPs in non-metropolitan areas may negatively impact the supply of urologic care providers and increase the disparity in access to care in non-metropolitan areas.
Source of Funding: None
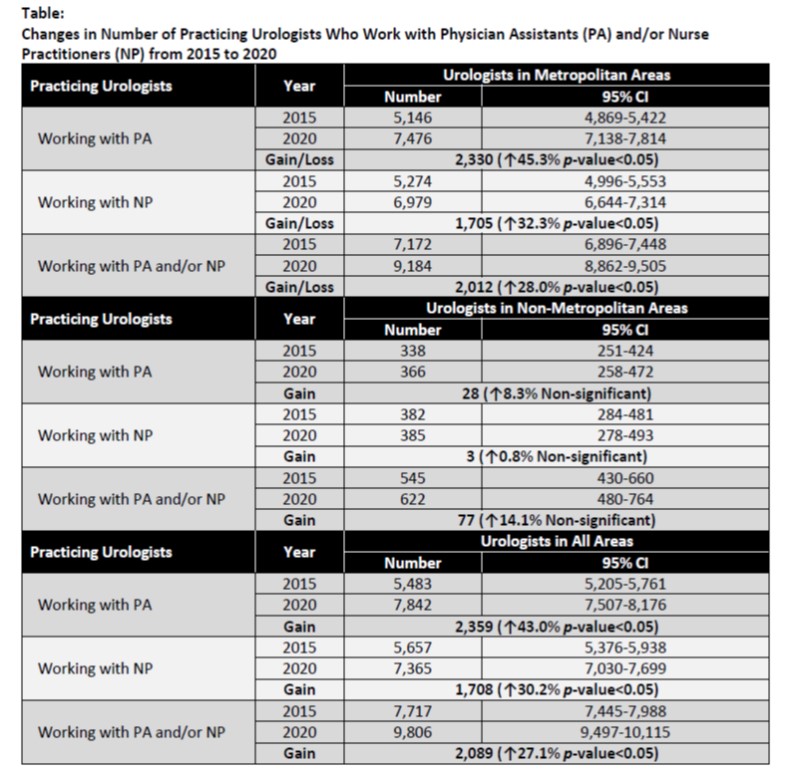
Methods: The American Urological Association (AUA) annual census data was used to compare APP growth rates from 2015 to 2020 in metropolitan and non-metropolitan areas in the United States. An area with a population size of 50,000 or more was defined as a metropolitan area. In contrast, an area with a population size under 50,000 was defined as a non-metropolitan area. Counts and growth rates of PAs and NPs or collectively APPs were calculated between 2015 and 2020.
Results: The number of practicing urologists who worked with physician assistants (PA) and nurse practitioners (NP) increased from 5,146 and 5,272 in 2015 to 7,476 and 6,979 in 2020. The growth rates of urologists who worked with PA and NP were much higher in metropolitan areas (45.3% and 32.3% or overall 28.0%) compared to non-metropolitan areas (8.3% and 0.8% or overall 14.1%) from 2015 to 2020.
Conclusions: There is a known shortage of urologists in rural counties and urologists who practice in rural areas are less likely to have APPs on staff. APPs are known to benefit urologic practices by reducing patient waiting times, improving overall productivity, and improving patient education. APPs may also serve a benefit in providing urologic care where there is no urologist. The number of practicing urologists working with APPs has increased over the past five years however there is a significant difference in the growth rate of urologists working with APPs in metropolitan areas than in non-metropolitan areas. The slower growth of urologists who worked with APPs in non-metropolitan areas may negatively impact the supply of urologic care providers and increase the disparity in access to care in non-metropolitan areas.
Source of Funding: None

.jpg)
.jpg)