Back
Poster, Podium & Video Sessions
Moderated Poster
MP41: Surgical Technology & Simulation: Training & Skills Assessment
MP41-11: Analysis of Flexible Ureteroscopic Motion and Kinematic Efficiency - A Simulation-based Pilot Study
Sunday, May 15, 2022
10:30 AM – 11:45 AM
Location: Room 228
Marie-Therese Valovska*, Gricelda Gomez, Boston, MA, Richard Fineman, William Woltmann, Cambridge, MA, Leia Stirling, Ann Arbor, MI, Daniel Wollin, Boston, MA

Marietherese Valovska, MD (she/her/hers)
Urology Resident
Brigham and Women's Hospital, Boston, MA
Poster Presenter(s)
Introduction: Flexible ureteroscopy (fURS) is the most common surgical procedure for treatment of urolithiasis. Various surgical disciplines and subspecialties have examined surgeon kinematics to improve assessment and generate measures of skill. Despite frequency of utilization, there is no undisputed method for evaluating fURS skills. Our pilot study utilized kinematic evaluations of fURS simulation to determine whether specific surgeon movements, techniques, and strategies correlate with measures of ureteroscopic efficiency.
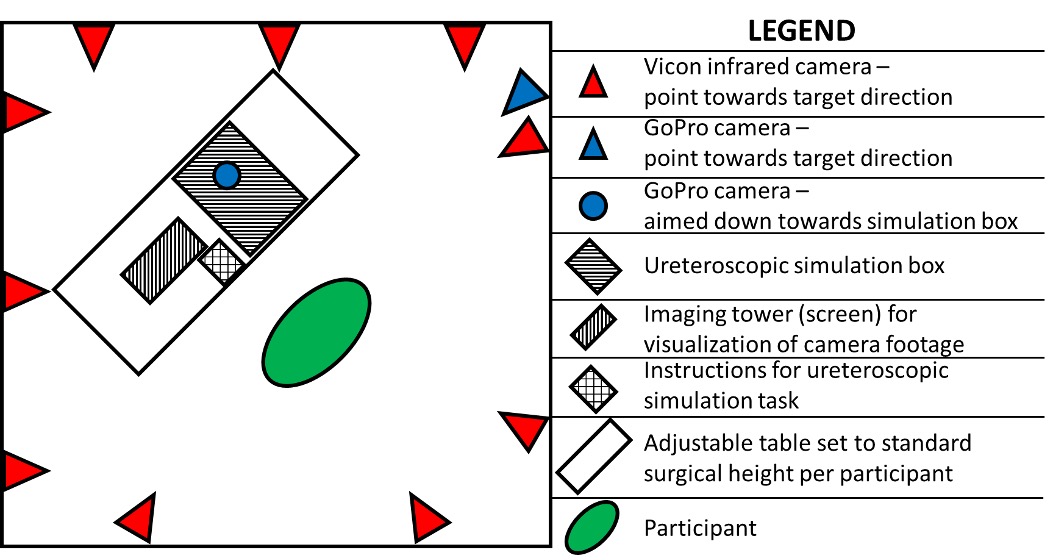
Methods: A motion capture system with 41 reflective markers and standard GoPro video camera were employed to characterize surgeon movement variables. A ureteroscopic simulation box was used by practicing urologists at various skill levels to perform a series of simple and complex ureteroscopic movement tasks. Two tasks were chosen for this initial pilot analysis. Body kinematics, time to task completion, and ureteroscopic movements were analyzed. Task efficiency was defined as quicker time to task completion and smaller ureteroscope end effector travel distance. A novel combined performance efficiency score (PES) was calculated using the root sum square of these two measures to characterize efficiency and skill.
Results: Twelve practicing urologists were enlisted. Average urologist age was 37 years with an average of 10.1 years of training; 50% were female, 50% were residents; and 33% had completed an Endourology fellowship. For the simple task, no kinematic data correlated with PES; for the complex task, participant head and torso movement correlated with PES (r=0.60, p=0.04 for head; r=0.65, p=0.02 for torso), with decreased body movement associated with higher efficiency.
Conclusions: Our findings suggest that movement economy measures are associated with efficient ureteroscopic manipulation for complex tasks in a simulated setting. Decreased head and torso movement were associated with higher efficiency, suggesting that excess body movement may signal extraneous or improper ureteroscopic movements. Additional assessment of these variables, including analysis in a clinical setting, is warranted as this may serve as a basis for improvement in endoscopic training and evaluation.
Source of Funding: The simulation box and single-use ureteroscopes were provided by Boston Scientific.
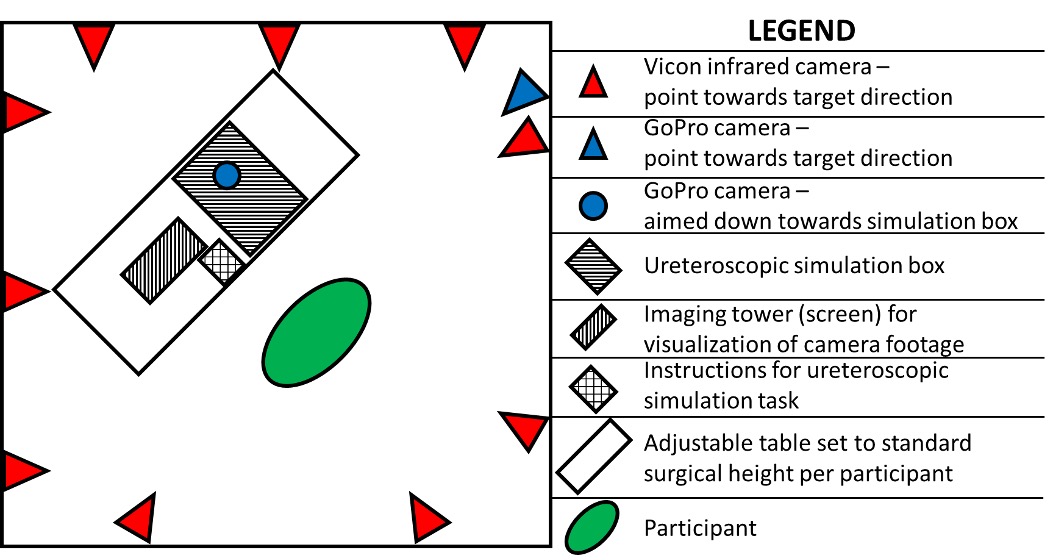
Methods: A motion capture system with 41 reflective markers and standard GoPro video camera were employed to characterize surgeon movement variables. A ureteroscopic simulation box was used by practicing urologists at various skill levels to perform a series of simple and complex ureteroscopic movement tasks. Two tasks were chosen for this initial pilot analysis. Body kinematics, time to task completion, and ureteroscopic movements were analyzed. Task efficiency was defined as quicker time to task completion and smaller ureteroscope end effector travel distance. A novel combined performance efficiency score (PES) was calculated using the root sum square of these two measures to characterize efficiency and skill.
Results: Twelve practicing urologists were enlisted. Average urologist age was 37 years with an average of 10.1 years of training; 50% were female, 50% were residents; and 33% had completed an Endourology fellowship. For the simple task, no kinematic data correlated with PES; for the complex task, participant head and torso movement correlated with PES (r=0.60, p=0.04 for head; r=0.65, p=0.02 for torso), with decreased body movement associated with higher efficiency.
Conclusions: Our findings suggest that movement economy measures are associated with efficient ureteroscopic manipulation for complex tasks in a simulated setting. Decreased head and torso movement were associated with higher efficiency, suggesting that excess body movement may signal extraneous or improper ureteroscopic movements. Additional assessment of these variables, including analysis in a clinical setting, is warranted as this may serve as a basis for improvement in endoscopic training and evaluation.
Source of Funding: The simulation box and single-use ureteroscopes were provided by Boston Scientific.

.jpg)
.jpg)