Back
Poster, Podium & Video Sessions
Moderated Poster
MP42: Bladder Cancer: Epidemiology & Evaluation II
MP42-04: Financial Burden of Bladder Cancer Care: CDC National Health Survey Analysis
Sunday, May 15, 2022
10:30 AM – 11:45 AM
Location: Room 225
Laura Bukavina*, Alberto Castro Bigalli, Philadelphia, PA, Thomas Cwalina, Caleb Curry, Michael Callegari, Megan Prunty, Ilaha Isali, Cleveland, OH, Mohit Sindhani, New Delhi, India, Adam Calaway, Lee Ponsky, Cleveland, OH, Andres Correa, Alexander Kutikov, Philadelphia, PA, Sarah Psutka, Seattle, WA
- LB
Poster Presenter(s)
Introduction: Financial toxicity (FT) has been associated with inferior clinical outcomes and is particularly relevant in bladder cancer (BCa). We aimed to analyze the impact of FT in BCa patients through measurement of the prevalence of delayed or missed clinical care secondary to FT.
Methods: We used 2008-2016 Centers for Disease Control National Health Interview Survey (CDC NHIS) to identify adults with history of BCa, stratified by age (18-64yo, >65yo) and compared them to adults without a history of cancer. We measured the following financial stressors 1) delaying or foregoing medical care 2) delay in dental care 3) worry about medical bills 4) delay in seeking mental health 5) difficulties paying for prescription medication. We used sampling and design variables to account for the complex survey design and participant nonresponse, and to make the estimates nationally representative. To estimate the association between covariates and BCa related problems, we used multivariable logistic regression (predictive margins).
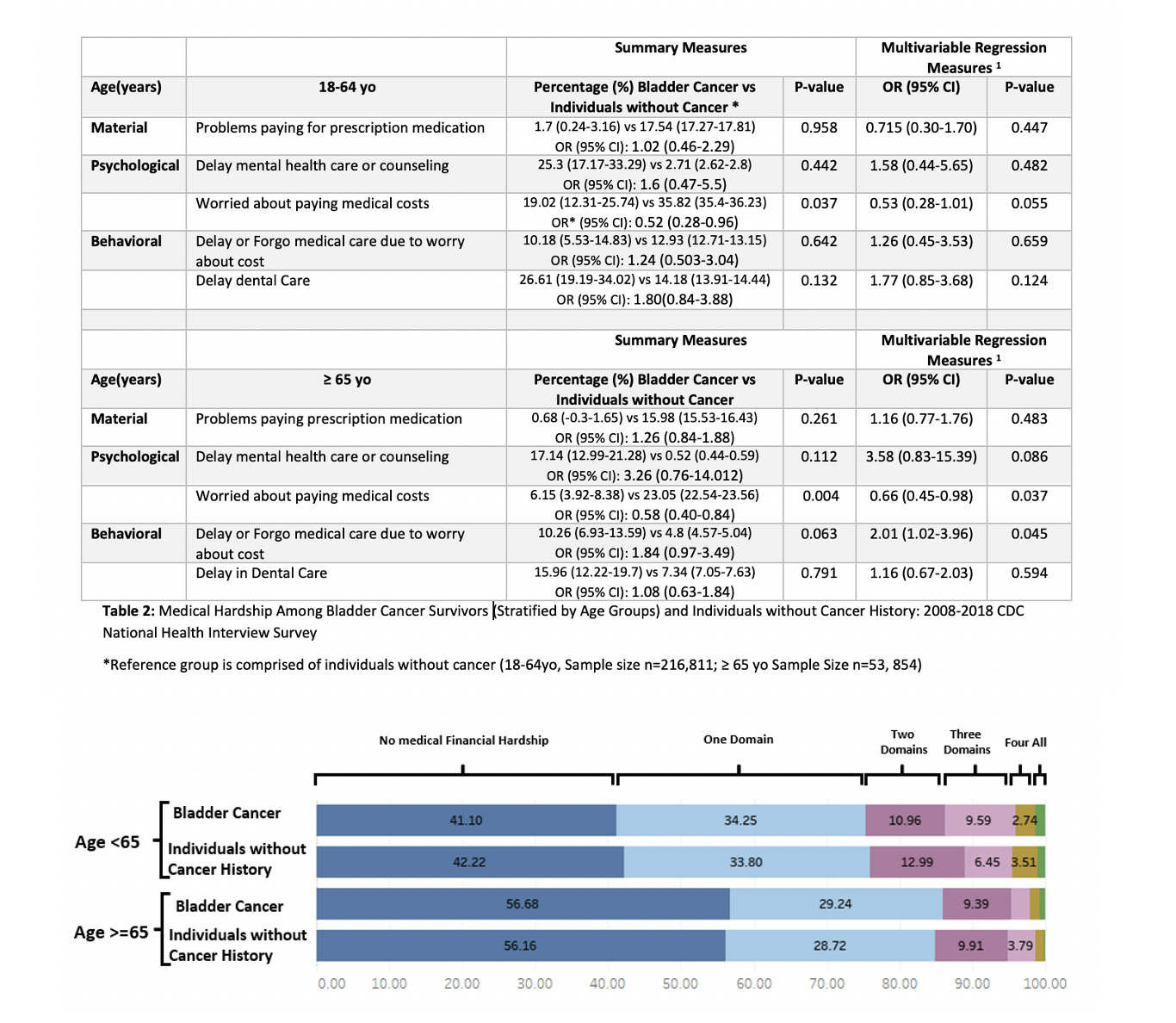
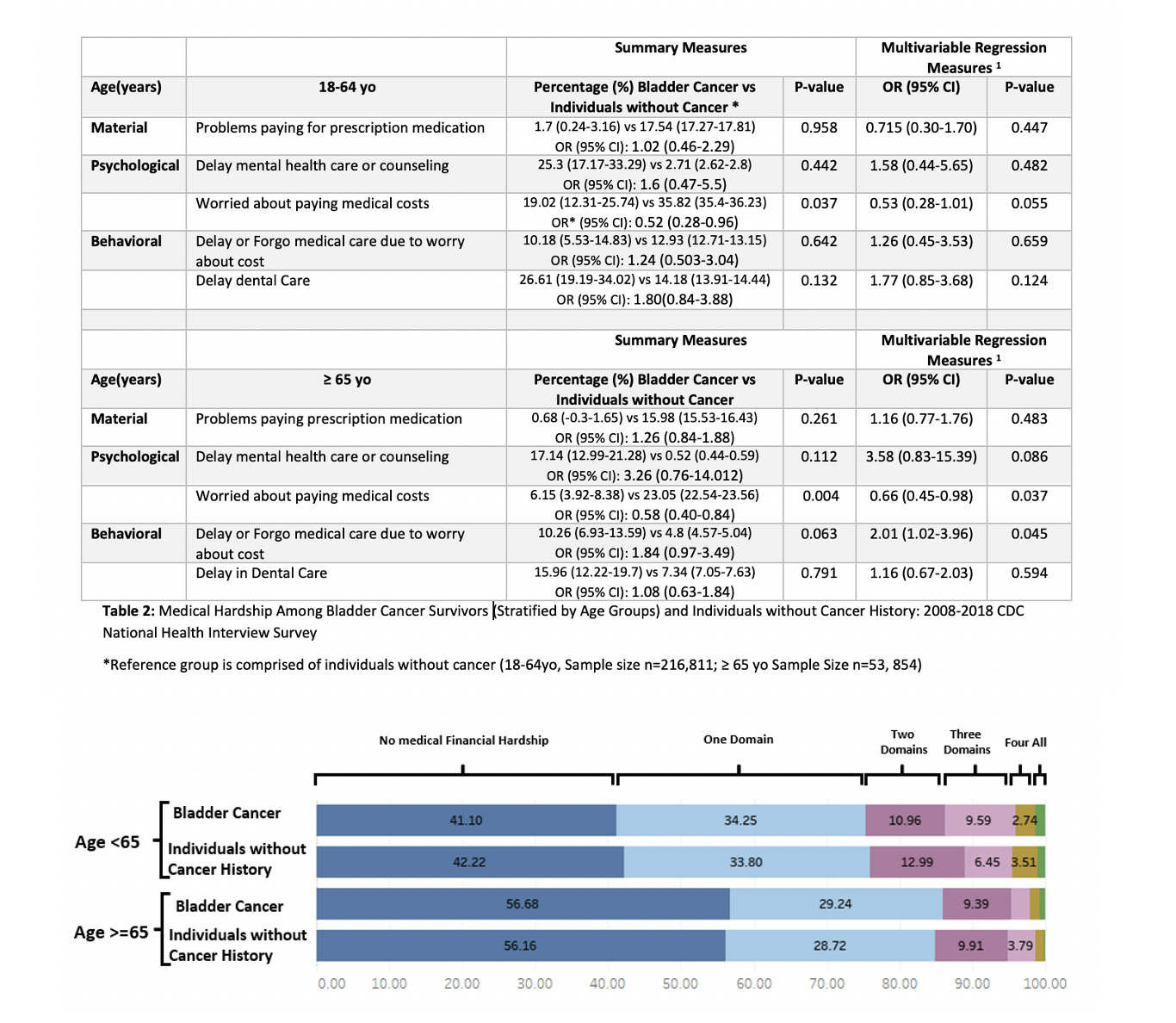
Results: BCa survivors (18-64yo) did not report higher incidence of delay in care or foregoing care, worrying about medical bills, or inability to afford prescription medication. BCa survivors (>65yo) reported higher incidence of inability to afford mental care (17.14% vs 0.52%), delaying or foregoing care (10.26% vs 4.8%). However, BCa patients did not report an increase in worry about paying for medical bills (6.15 % vs 23.05%), and inability to afford prescriptions (0.68 vs 15.98%). On multivariable analysis, the odds ratio of individual measures reported highlighted that BCa survivors were less likely to report worrying about medical costs [OR 0.66, p=0.037]as compared to individuals without cancer (after adjusting for clinical characteristics and comorbidities), although they were more likely to report delay in medical care [OR 1.16, p=0.045]. (Table 2)
Conclusions: Identification of patients at risk for excess medical financial hardships is needed to move the discussion from problem acknowledgement to identifying solutions and implementing strategies.
Source of Funding: None
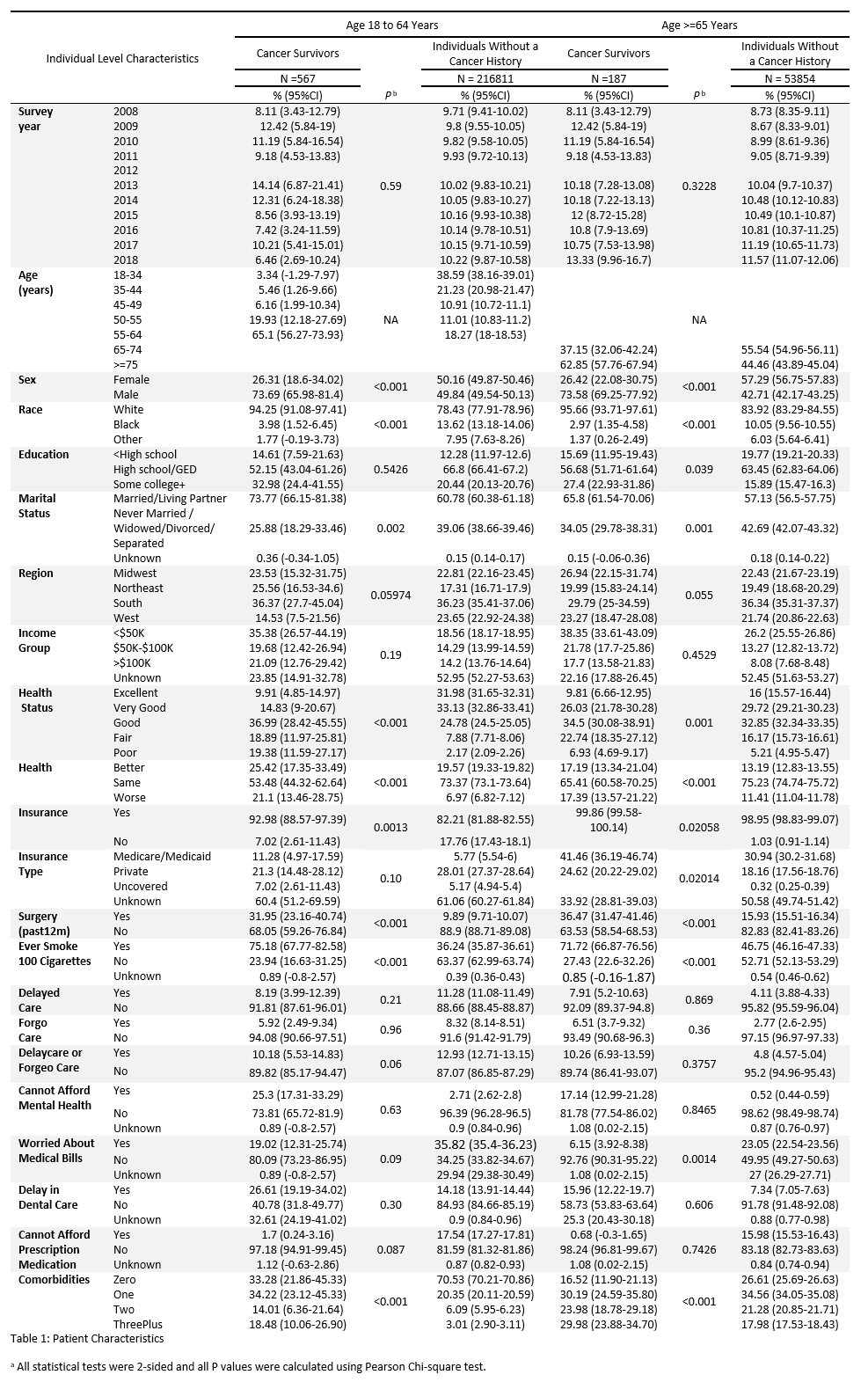
Methods: We used 2008-2016 Centers for Disease Control National Health Interview Survey (CDC NHIS) to identify adults with history of BCa, stratified by age (18-64yo, >65yo) and compared them to adults without a history of cancer. We measured the following financial stressors 1) delaying or foregoing medical care 2) delay in dental care 3) worry about medical bills 4) delay in seeking mental health 5) difficulties paying for prescription medication. We used sampling and design variables to account for the complex survey design and participant nonresponse, and to make the estimates nationally representative. To estimate the association between covariates and BCa related problems, we used multivariable logistic regression (predictive margins).
Results: BCa survivors (18-64yo) did not report higher incidence of delay in care or foregoing care, worrying about medical bills, or inability to afford prescription medication. BCa survivors (>65yo) reported higher incidence of inability to afford mental care (17.14% vs 0.52%), delaying or foregoing care (10.26% vs 4.8%). However, BCa patients did not report an increase in worry about paying for medical bills (6.15 % vs 23.05%), and inability to afford prescriptions (0.68 vs 15.98%). On multivariable analysis, the odds ratio of individual measures reported highlighted that BCa survivors were less likely to report worrying about medical costs [OR 0.66, p=0.037]as compared to individuals without cancer (after adjusting for clinical characteristics and comorbidities), although they were more likely to report delay in medical care [OR 1.16, p=0.045]. (Table 2)
Conclusions: Identification of patients at risk for excess medical financial hardships is needed to move the discussion from problem acknowledgement to identifying solutions and implementing strategies.
Source of Funding: None

.jpg)
.jpg)