Back
Poster, Podium & Video Sessions
Moderated Poster
MP53: Prostate Cancer: Detection & Screening V
MP53-20: Added value of mpMRI in the stratification of patients with High-Risk Patients Prostate Cancer treated with radical prostatectomy: Implications for tailored multi-modal strategies.
Monday, May 16, 2022
7:00 AM – 8:15 AM
Location: Room 225
Giuseppe Cirulli*, Milan, Italy, Elio Mazzone, Milano, Italy, Giorgio Gandaglia, Milan, Italy, Razvan-George Rahota, Toulouse, France, Giancarlo Marra, Turin, Italy, Massimo Valerio, Lausanne, Switzerland, Riccardo Campi, Andrea Mari, Florence, Italy, Agostino Mattei, Marco Moschini, Lucerne, Switzerland, Jean Baptiste Beauval, Mathieu Roumiguiè, Toulouse, France, Luca Afferi, Lucerne, Italy, Paolo Gontero, Turin, Italy, Armando Stabile, Milan, Italy, Nicola Fossati, Lugano, Switzerland, Vito Cucchiara, Giuseppe Rosiello, Francesco Montorsi, Alberto Briganti, Milan, Italy
- GC
Poster Presenter(s)
Introduction: In patients with high-risk prostate cancer, it is unclear whether multiparametric MRI (mpMRI) adds value for the identification of patients at higher risk of early biochemical recurrence (BCR) who may be candidates to receive multi-modal therapy. Therefore, we tested whether MRI parameters may predict outcomes in high-risk patients.
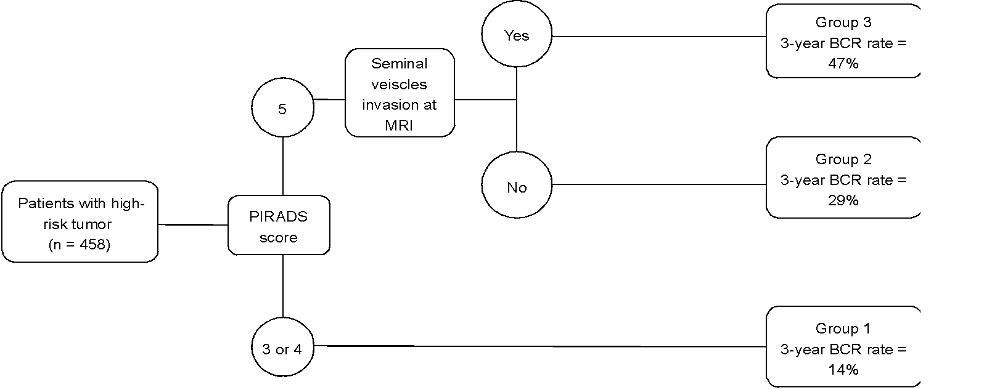
Methods: We relied on 458 patients classified as high-risk according to clinical risk factors (i.e. PSA >20 ng/ml or cT3 or biopsy Grade group (GG) 4-5) and treated with RP between 2015 and 2020 at seven centres. The outcome was BCR defined as two PSA =0.2 ng/ml after RP. Multivariable Cox regressions (MVA) tested MRI-based predictors of BCR. Predictors were PIRADS (3 vs 4 vs 5), max diameter of the index lesion (IL) and MRI stage (organ-confined vs extracapsular extension [ECE] vs. seminal vesicles invasion [SVI]). Regression tree analysis stratified patients into risk groups for 3-year BCR according to mpMRI data. We also compared the accuracy of novel MRI-based risk categories to a previously validated clinical stratification: a good prognosis group (one high-risk factor); an intermediate prognosis group (PSA >20 ng/ml and cT3); and a poor prognosis group (GG 4–5 with at least one other high-risk factor)
Results: Median follow-up was 34 months. Overall, 115 (25%), 103 (22%) and 325 (71%) patients had PSA = 20, cT3 disease and GG 4-5. 236 (51%) and 42 (9%) patients had PIRADS 5 lesions and SVI at MRI. Median max diameter of the IL was 12 mm. The 3-year BCR-free survival was 70%. At MVA, PIRADS 5 (HR 3.14, p=0.008) and SVI at MRI (HR 2.41, p=0.002) correlated with higher risk of BCR, while higher IL diameter did not (HR 0.99, p=0.1). At regression tree analysis, patients were stratified in three risk groups according to PIRADS and MRI stage (Figure 1). This model depicted good discrimination for BCR (AUC 76%) which outperformed the accuracy of the categorization based on clinical risk factors only (AUC 63%).
Conclusions: Preoperative mpMRI can optimize the identification of high-risk patients for early BCR. Men with PIRADS 4 or 5 lesions and suspected SVI at MRI experience early BCR in roughly 50% of the cases and should, therefore, be counselled on the non-negligible need for additional therapies within the first 3 years after RP.
Source of Funding: none
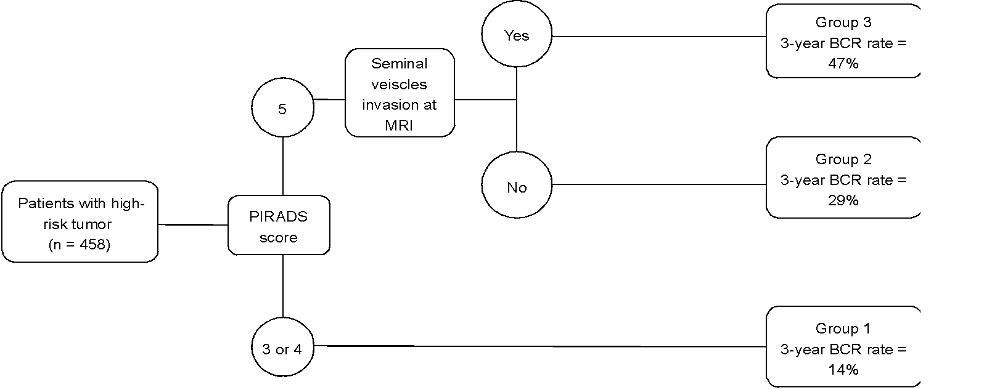
Methods: We relied on 458 patients classified as high-risk according to clinical risk factors (i.e. PSA >20 ng/ml or cT3 or biopsy Grade group (GG) 4-5) and treated with RP between 2015 and 2020 at seven centres. The outcome was BCR defined as two PSA =0.2 ng/ml after RP. Multivariable Cox regressions (MVA) tested MRI-based predictors of BCR. Predictors were PIRADS (3 vs 4 vs 5), max diameter of the index lesion (IL) and MRI stage (organ-confined vs extracapsular extension [ECE] vs. seminal vesicles invasion [SVI]). Regression tree analysis stratified patients into risk groups for 3-year BCR according to mpMRI data. We also compared the accuracy of novel MRI-based risk categories to a previously validated clinical stratification: a good prognosis group (one high-risk factor); an intermediate prognosis group (PSA >20 ng/ml and cT3); and a poor prognosis group (GG 4–5 with at least one other high-risk factor)
Results: Median follow-up was 34 months. Overall, 115 (25%), 103 (22%) and 325 (71%) patients had PSA = 20, cT3 disease and GG 4-5. 236 (51%) and 42 (9%) patients had PIRADS 5 lesions and SVI at MRI. Median max diameter of the IL was 12 mm. The 3-year BCR-free survival was 70%. At MVA, PIRADS 5 (HR 3.14, p=0.008) and SVI at MRI (HR 2.41, p=0.002) correlated with higher risk of BCR, while higher IL diameter did not (HR 0.99, p=0.1). At regression tree analysis, patients were stratified in three risk groups according to PIRADS and MRI stage (Figure 1). This model depicted good discrimination for BCR (AUC 76%) which outperformed the accuracy of the categorization based on clinical risk factors only (AUC 63%).
Conclusions: Preoperative mpMRI can optimize the identification of high-risk patients for early BCR. Men with PIRADS 4 or 5 lesions and suspected SVI at MRI experience early BCR in roughly 50% of the cases and should, therefore, be counselled on the non-negligible need for additional therapies within the first 3 years after RP.
Source of Funding: none

.jpg)
.jpg)