Back
Poster, Podium & Video Sessions
Moderated Poster
MP55: Prostate Cancer: Localized: Ablative Therapy
MP55-16: Focal Cryotherapy and Stereotactic Body Radiotherapy Have Similar Oncologic and Functional Outcomes in Treatment of Low-to-Intermediate Unilobe Prostate Cancer
Monday, May 16, 2022
8:45 AM – 10:00 AM
Location: Room 225
Ashley Monaco*, Glen Head, NY, Jessica Sommer, Garden City, NY, Chinyere Okpara, Jonathan Haas, Mineola, NY, Anthony Corcoran, Aaron Katz, Garden City, NY

Ashley Monaco, BS
New York Institute of Technology College of Osteopathic Medicine
Poster Presenter(s)
Introduction: Minimal invasive treatment options such as focal cryotherapy (FC) and stereotactic body radiotherapy (SBRT) continue to evolve and grow in popularity. Comparative outcome data for these treatment options are sparse. This study compares oncologic and functional outcomes as well as complications following FC or SBRT for low-to-intermediate risk unilobe prostate cancer (PCa).
Methods: An IRB-approved database was reviewed for patients who underwent FC or SBRT for low-to-intermediate risk PCa as defined by D’Amico criteria. Patients with >1 year of follow-up, had prior PCa treatment, or PCa that was bilateral were excluded from this study. TF was defined as salvage treatment, a positive biopsy Gleason group (GG) of 2 or greater on post-treatment biopsy, or PCa metastasis. Functional outcomes were based on 2-year post treatment patient reported EPIC urinary, sexual, and bowel function surveys. Complications were categorized with the Clavien Dindo classification (CD). Descriptive statistics, univariate analyses, and Kaplan Meier curve were used to compare outcomes of SBRT and FC. P<0.05 was significant.
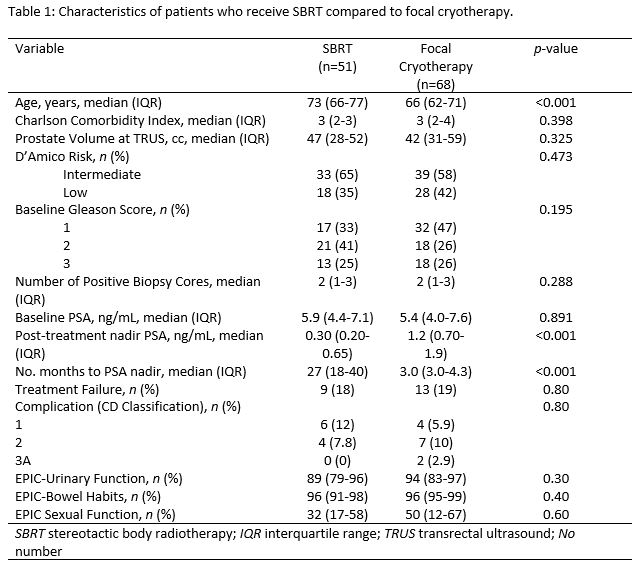
Results: 68 FC and 51 SBRT patients with a median age of 68 years (48-86) and a median follow-up time of 82 (14-135) months were included in this analysis. There was no difference in PCa risk (p=0.473), GG (p=0.2), or PSA (p=0.8) among the two cohorts at baseline. There was no difference between patients who experienced TF (19% vs. 18%; p=0.8; log-rank p=0.7), underwent salvage treatment (18% vs 18%; p=1.0), or had metastasis (2.9% vs. 9.8%; p=0.1) among FC and SBRT patients, respectively. At a minimum of 2-years post-treatment, urinary function (94 vs. 89; p=0.3), bowel function (96 vs. 96; p=0.4), and sexual function (50 vs. 32; p=0.6) were relatively similar among the FC and SBRT patients, respectively. 13 (19%) FC and 10 (20%) SBRT experienced treatment related complications (p=0.8) of which 4 (5.9%) FC and 6 (12%) were CD 1, 7 (10%) FC and 4 (7.8%) SBRT were CD 2, and 2 (2.9%) FC were CD 3A.
Conclusions: Both FC and SBRT are associated with similar, excellent oncologic and functional outcomes 7-years following treatment. These results underscore the utility of FC and SBRT for management of unilobe low-to-intermediate risk PCa.
Source of Funding: Department of Urology, NYU Langone Hospital – Long Island
Methods: An IRB-approved database was reviewed for patients who underwent FC or SBRT for low-to-intermediate risk PCa as defined by D’Amico criteria. Patients with >1 year of follow-up, had prior PCa treatment, or PCa that was bilateral were excluded from this study. TF was defined as salvage treatment, a positive biopsy Gleason group (GG) of 2 or greater on post-treatment biopsy, or PCa metastasis. Functional outcomes were based on 2-year post treatment patient reported EPIC urinary, sexual, and bowel function surveys. Complications were categorized with the Clavien Dindo classification (CD). Descriptive statistics, univariate analyses, and Kaplan Meier curve were used to compare outcomes of SBRT and FC. P<0.05 was significant.
Results: 68 FC and 51 SBRT patients with a median age of 68 years (48-86) and a median follow-up time of 82 (14-135) months were included in this analysis. There was no difference in PCa risk (p=0.473), GG (p=0.2), or PSA (p=0.8) among the two cohorts at baseline. There was no difference between patients who experienced TF (19% vs. 18%; p=0.8; log-rank p=0.7), underwent salvage treatment (18% vs 18%; p=1.0), or had metastasis (2.9% vs. 9.8%; p=0.1) among FC and SBRT patients, respectively. At a minimum of 2-years post-treatment, urinary function (94 vs. 89; p=0.3), bowel function (96 vs. 96; p=0.4), and sexual function (50 vs. 32; p=0.6) were relatively similar among the FC and SBRT patients, respectively. 13 (19%) FC and 10 (20%) SBRT experienced treatment related complications (p=0.8) of which 4 (5.9%) FC and 6 (12%) were CD 1, 7 (10%) FC and 4 (7.8%) SBRT were CD 2, and 2 (2.9%) FC were CD 3A.
Conclusions: Both FC and SBRT are associated with similar, excellent oncologic and functional outcomes 7-years following treatment. These results underscore the utility of FC and SBRT for management of unilobe low-to-intermediate risk PCa.
Source of Funding: Department of Urology, NYU Langone Hospital – Long Island

.jpg)
.jpg)