Back
Poster, Podium & Video Sessions
Podium
PD02: Pediatric Urology: Neurogenic Bladder, Reconstruction & DSD
PD02-01: Prenatal Closure of Myelomeningocele is Associated with Higher Risk for Early Secondary Spinal Cord Tethering
Friday, May 13, 2022
7:00 AM – 7:10 AM
Location: Room 255
Hsin-Hsiao Wang*, Duncan Morhardt, Benjamin Warf, Lawrence Karlin, Asal Hojjat, Shahram Khoshbin, Erin Mcnamara, Carlos Estrada, Stuart Bauer, Boston, MA
- HW
Podium Presenter(s)
Introduction: The long-term impact of prenatal myelomeningocele (MMC) closure on neuro-urologic function is unclear. Urodynamic studies (UDS) often serve as an early indicator of symptomatically acquired spinal cord tethering. We sought to compare the risk for early neuro-urologic deterioration due to spinal cord tethering in children with prenatal versus postnatal MMC repair.
Methods: Children with prenatal MMC closure followed at our institution from 1999 to 2019 were included. Children with postnatally closed MMC were selected as matched controls in 1:3 ratio by sex, neurological level, & follow-up. Primary outcome was defined as time to secondary untethering procedure. Birth year, gender, functional neurological level, UDS & reasons for surgery were assessed. Multivariate cox proportional hazard model was fitted.
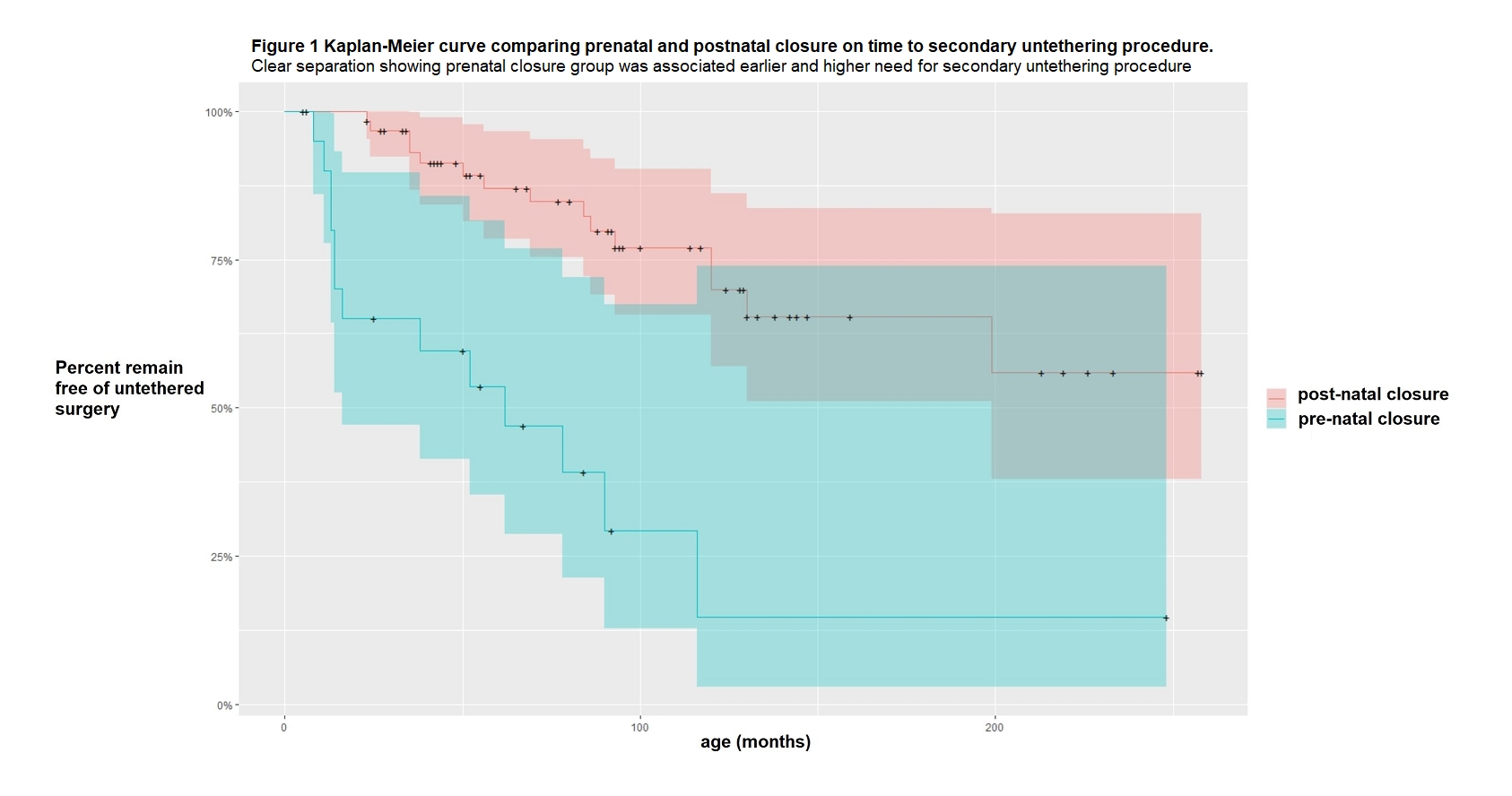
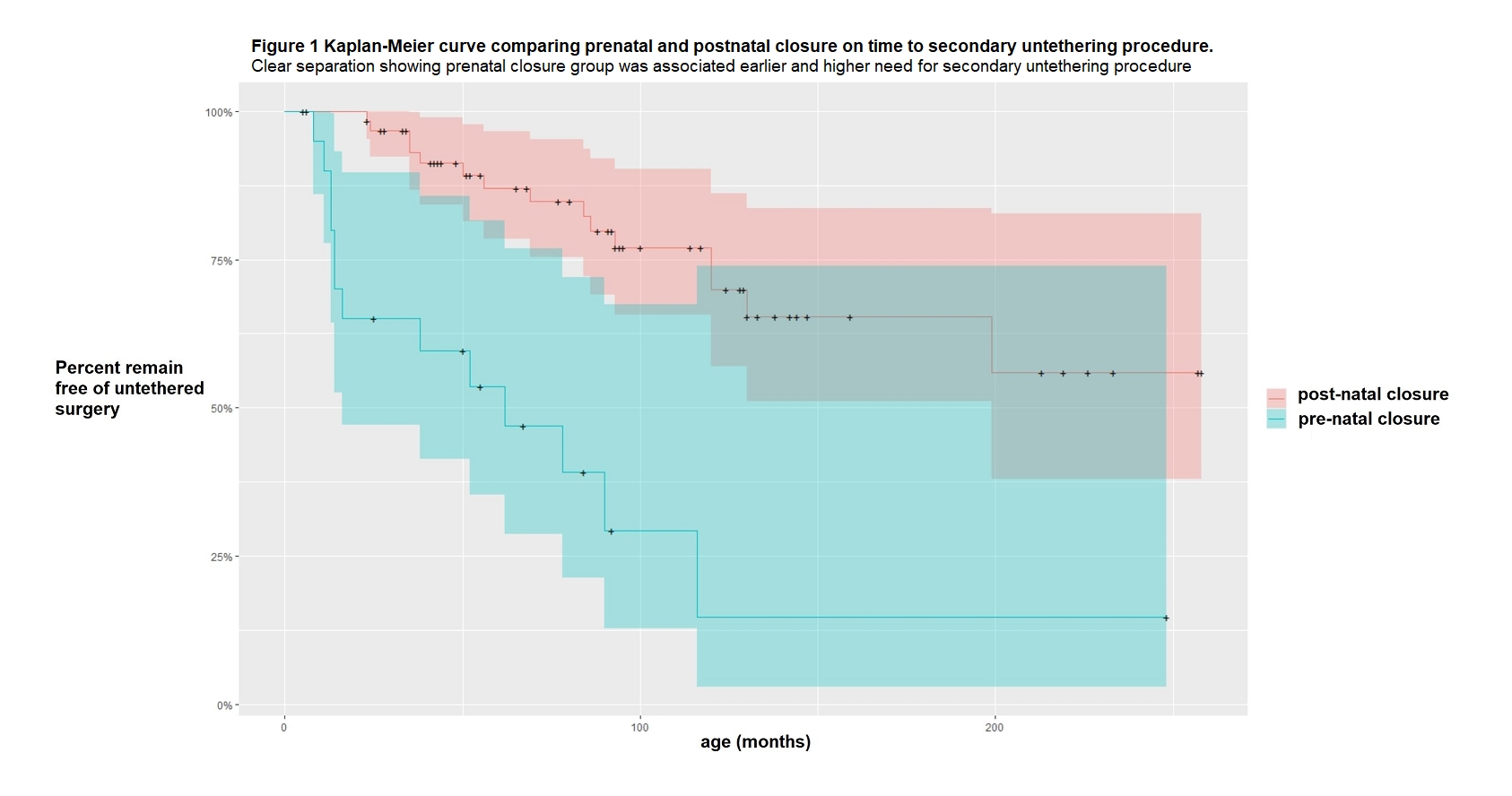
Results: Our study included 21 with prenatal & 62 with postnatal MMC closure. 12/21 (57%) of the prenatally and 15/62 (24%) of the postnatally closed babies underwent secondary spinal cord surgery (SSCS). Median age for SSCS in those closed prenatal was younger (median 16 [IQR 13-62] months) compared to the postnatal group (median 69 [IQR 35-120] months, p=0.02). Compared to the postnatal MMC group, prenatal MMC closure was significantly associated with need for SSCS (p < 0.01, figure 1). When adjusting for birth year, sex, functional neurologic level, prenatal MMC closure remained significantly associated with the need for untethering surgery (HR=4.7(2.5-12.0), p<0.001). Under the same MMC bladder management protocol for both groups, 8/12 (67%) of prenatally closed children requiring secondary untethering surgery had symptomatic UDS changes, with 7/8 (88%) showing improved postoperative UDS parameters. Similarly, 93% (14/15) of postnatally closed children with acquired tethering had UDS changes, with 11/14 (78%) showing improved postoperative UDS.
Conclusions: We found substantially more children with prenatal MMC closure who required SSCS compared to those closed postnatally. In each group, most presented with worsening UDS parameters. Early detection of UDS changes & secondary untethering resulted in neuro-urologic improvement. The cause of this phenomenon is not clear and requires further investigation.
Source of Funding: none
Methods: Children with prenatal MMC closure followed at our institution from 1999 to 2019 were included. Children with postnatally closed MMC were selected as matched controls in 1:3 ratio by sex, neurological level, & follow-up. Primary outcome was defined as time to secondary untethering procedure. Birth year, gender, functional neurological level, UDS & reasons for surgery were assessed. Multivariate cox proportional hazard model was fitted.
Results: Our study included 21 with prenatal & 62 with postnatal MMC closure. 12/21 (57%) of the prenatally and 15/62 (24%) of the postnatally closed babies underwent secondary spinal cord surgery (SSCS). Median age for SSCS in those closed prenatal was younger (median 16 [IQR 13-62] months) compared to the postnatal group (median 69 [IQR 35-120] months, p=0.02). Compared to the postnatal MMC group, prenatal MMC closure was significantly associated with need for SSCS (p < 0.01, figure 1). When adjusting for birth year, sex, functional neurologic level, prenatal MMC closure remained significantly associated with the need for untethering surgery (HR=4.7(2.5-12.0), p<0.001). Under the same MMC bladder management protocol for both groups, 8/12 (67%) of prenatally closed children requiring secondary untethering surgery had symptomatic UDS changes, with 7/8 (88%) showing improved postoperative UDS parameters. Similarly, 93% (14/15) of postnatally closed children with acquired tethering had UDS changes, with 11/14 (78%) showing improved postoperative UDS.
Conclusions: We found substantially more children with prenatal MMC closure who required SSCS compared to those closed postnatally. In each group, most presented with worsening UDS parameters. Early detection of UDS changes & secondary untethering resulted in neuro-urologic improvement. The cause of this phenomenon is not clear and requires further investigation.
Source of Funding: none

.jpg)
.jpg)