Back
Poster, Podium & Video Sessions
Podium
PD14: Bladder Cancer: Epidemiology & Evaluation I
PD14-11: Use of a Physical Activity Monitor to Track Perioperative Activity of Radical Cystectomy Patients: Our First Glimpse at What Our Patients are Really Doing Before and After Surgery
Friday, May 13, 2022
5:10 PM – 5:20 PM
Location: Room 255
Alex Zhu, DO*, Joel Berends, MD, Stephanie Daignault-Newton, MS, Ann Arbor, MI, Deborah Kaye, MD, Durham, NC, Christine Schafer, BS, Steven Thelen-Perry, BS, Chrissy Parker, MS, Heidi Iglay-Reger, PhD, Yongmei Qin, MD, Todd M. Morgan, MD, Alon Z. Weizer, MD, Samuel D. Kaffenberger, MD, Lindsey A. Herrel, MD, Khaled Hafez, MD, Ann Arbor, MI, Cheryl T. Lee, MD, Columbus, OH, Ted A. Skolarus, MD, Michael Englesbe, MD, Jeffrey S. Montgomery, MD, Ann Arbor, MI
- AZ
Podium Presenter(s)
Introduction: Radical cystectomy (RC) is a morbid procedure with high complication and readmission rates. To optimize recovery, providers stress the importance of early ambulation and adequate rest. However, little is known about the activity and sleep habits of patients undergoing RC. We utilized a wearable physical activity monitor (PAM) to track patients during the perioperative period. Our aim is to provide the first objective activity data for RC patients.
Methods: We prospectively identified patients >59 years old with planned RC. Participants completed a 4-week prehabilitation exercise program prior to surgery. They wore a PAM for seven day intervals: at baseline, after completing prehabilitation, at postoperative day (POD) 30 and POD 90. Patients wore the PAM for a minimum of 22 hours/day for inclusion.
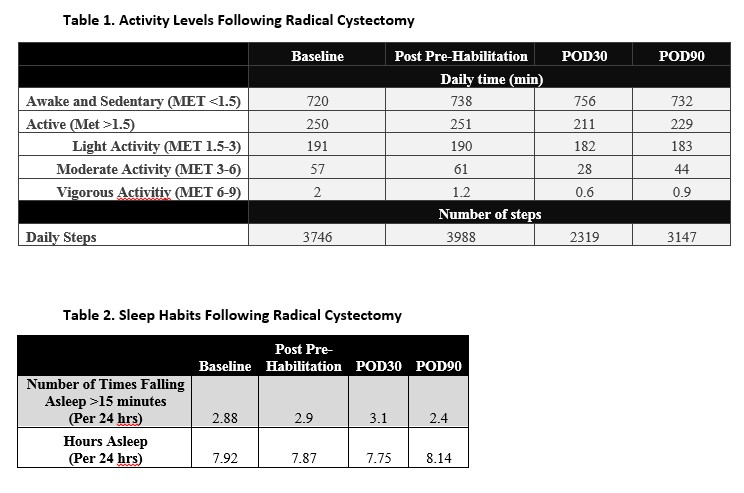
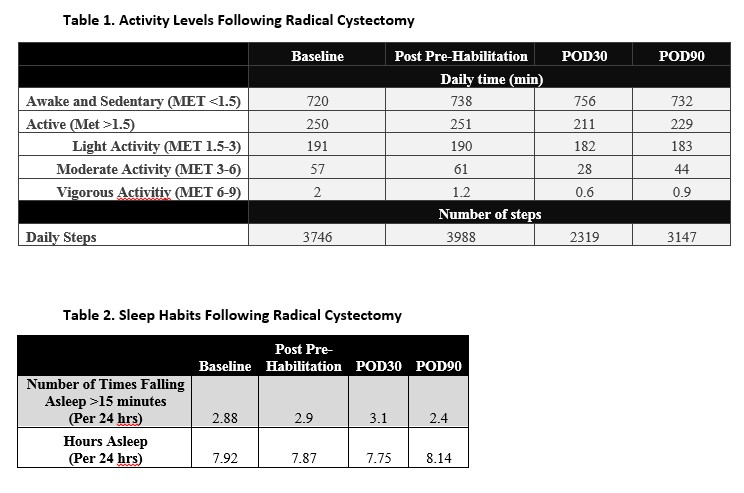
We tracked physical activity via metabolic equivalents (METs). We found the time patients were active (MET>1.5), and sedentary but awake (MET <1.5). We calculated time spent performing light (MET 1.5-3), moderate (MET 3-6) and vigorous activities (MET 6-9). We calculated daily number of steps. We tracked total hours of sleep and number of times patients fell asleep (minimum > 15 minutes).
Results: 42 patients underwent RC and met inclusion criteria. On average, patients wore the PAM for 23.5 hours/day.
Physical activity levels and sleep patterns are described (Table 1, 2). The ability to perform light activities, such as activities of daily living, were not hampered in a clinically significant manner after RC. Patients were only sedentary an additional 36 and 12 minutes at POD30 and POD90, respectively, compared to baseline. Moderate and vigorous activities, as well as number of steps were substantially decreased following RC. Patients slept the least and had the most fragmented sleep at POD30. Conversely, patients slept the most with the least fragmentation at POD90.
Conclusions: This is the first study to utilize physical activity monitors to track activity and sleep habits of patients undergoing RC. This study gives patients and providers a better understanding of post-cystectomy recovery expectations. With these results in mind, interventions may be implemented to optimize patient activity and sleep in the perioperative period.
Source of Funding: N/A
Methods: We prospectively identified patients >59 years old with planned RC. Participants completed a 4-week prehabilitation exercise program prior to surgery. They wore a PAM for seven day intervals: at baseline, after completing prehabilitation, at postoperative day (POD) 30 and POD 90. Patients wore the PAM for a minimum of 22 hours/day for inclusion.
We tracked physical activity via metabolic equivalents (METs). We found the time patients were active (MET>1.5), and sedentary but awake (MET <1.5). We calculated time spent performing light (MET 1.5-3), moderate (MET 3-6) and vigorous activities (MET 6-9). We calculated daily number of steps. We tracked total hours of sleep and number of times patients fell asleep (minimum > 15 minutes).
Results: 42 patients underwent RC and met inclusion criteria. On average, patients wore the PAM for 23.5 hours/day.
Physical activity levels and sleep patterns are described (Table 1, 2). The ability to perform light activities, such as activities of daily living, were not hampered in a clinically significant manner after RC. Patients were only sedentary an additional 36 and 12 minutes at POD30 and POD90, respectively, compared to baseline. Moderate and vigorous activities, as well as number of steps were substantially decreased following RC. Patients slept the least and had the most fragmented sleep at POD30. Conversely, patients slept the most with the least fragmentation at POD90.
Conclusions: This is the first study to utilize physical activity monitors to track activity and sleep habits of patients undergoing RC. This study gives patients and providers a better understanding of post-cystectomy recovery expectations. With these results in mind, interventions may be implemented to optimize patient activity and sleep in the perioperative period.
Source of Funding: N/A

.jpg)
.jpg)