Back
Poster, Podium & Video Sessions
Podium
PD22: Prostate Cancer: Localized: Radiation Therapy
PD22-03: Urinary Function Following High Dose Intensity Modulated Radiotherapy for Clinically Localized Prostate Cancer
Saturday, May 14, 2022
9:50 AM – 10:00 AM
Location: Room 252
Shannon McNall*, Nathan Colin Wong, Valhalla, NY, Shawn Zimberg, John Rescigno, Hartsdale, NY
- SM
Podium Presenter(s)
Introduction: Approximately 1/3 of men undergoing treatment for prostate cancer in the U.S. receive external beam radiotherapy (RT). The International Prostate Symptom Score (IPSS) is a validated tool that assesses urinary function. We assessed pre- and post-RT IPSS in a large cohort of men treated with RT + androgen deprivation therapy (ADT) for clinically localized prostate cancer and examined factors associated with baseline IPSS and worsening IPSS after RT.
Methods: Patients treated with intensity modulated RT at Advanced Radiation Centers of New York from 2006 to 2017 were included. IMRT total dose to the prostate was 81-86Gy in 45-48 fractions/9-10 weeks. High-risk patients were treated with ADT + pelvic lymph node RT to 45Gy. Paired samples t-test with bootstrapping was used for comparison of pre- and post-treatment IPSS (mean + 95% CI). Factors associated with IPSS were evaluated using crosstab analysis and Pearson chi-square. Those significant with p<0.05 were evaluated in multivariate analysis using binary logistic regression. Factors assessed were age, T stage, grade group, NCCN risk group, perineural invasion, >50% cores positive, use of ADT, and use of pelvic lymph node RT.
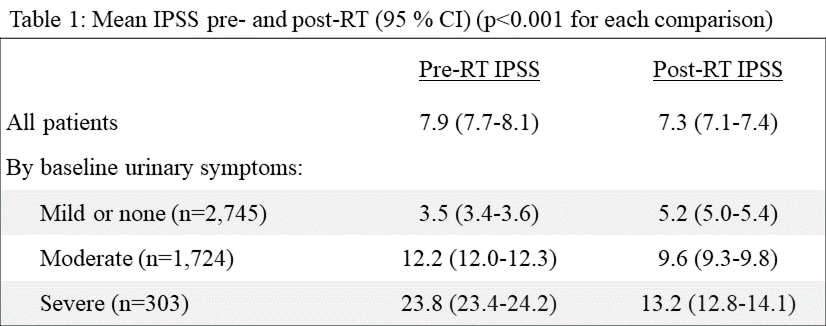
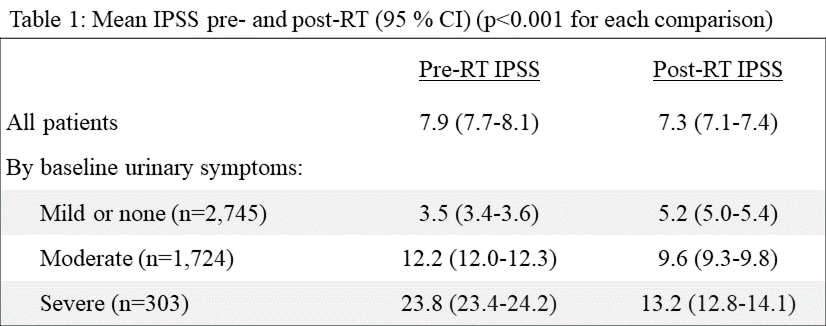
Results: 4,772 men had baseline IPSS prior to RT and 6-18 months post-RT (mean 11.8, median 13.1). Overall, there was minor improvement in urinary function post-RT (p < 0.001). When assessed by baseline urinary function, the improvement was clinically significant for those with severe baseline urinary symptoms (Table 1). Association between age and baseline IPSS was significant. Moderate/severe baseline urinary symptoms (pre-RT IPSS > 20) were present in 44% of men >60 years and 36% of men <60 (p < 0.001). Worsened urinary function after RT was associated with pelvic lymph node RT: 44% vs. 40% (p=0.02). Moderate/severe post-RT urinary function was present in 45% of men who received pelvic lymph node RT vs. 37% of those who did not (p < 0.001).
Conclusions: Men with localized prostate cancer and baseline moderate/severe urinary symptoms had improved urinary function 6-18 months post-RT, while those with mild urinary symptoms had a modest worsening of symptoms. RT to the pelvic lymph nodes was independently associated with a worsened one-year urinary function score. These data can help inform patient expectations following RT.
Source of Funding: None
Methods: Patients treated with intensity modulated RT at Advanced Radiation Centers of New York from 2006 to 2017 were included. IMRT total dose to the prostate was 81-86Gy in 45-48 fractions/9-10 weeks. High-risk patients were treated with ADT + pelvic lymph node RT to 45Gy. Paired samples t-test with bootstrapping was used for comparison of pre- and post-treatment IPSS (mean + 95% CI). Factors associated with IPSS were evaluated using crosstab analysis and Pearson chi-square. Those significant with p<0.05 were evaluated in multivariate analysis using binary logistic regression. Factors assessed were age, T stage, grade group, NCCN risk group, perineural invasion, >50% cores positive, use of ADT, and use of pelvic lymph node RT.
Results: 4,772 men had baseline IPSS prior to RT and 6-18 months post-RT (mean 11.8, median 13.1). Overall, there was minor improvement in urinary function post-RT (p < 0.001). When assessed by baseline urinary function, the improvement was clinically significant for those with severe baseline urinary symptoms (Table 1). Association between age and baseline IPSS was significant. Moderate/severe baseline urinary symptoms (pre-RT IPSS > 20) were present in 44% of men >60 years and 36% of men <60 (p < 0.001). Worsened urinary function after RT was associated with pelvic lymph node RT: 44% vs. 40% (p=0.02). Moderate/severe post-RT urinary function was present in 45% of men who received pelvic lymph node RT vs. 37% of those who did not (p < 0.001).
Conclusions: Men with localized prostate cancer and baseline moderate/severe urinary symptoms had improved urinary function 6-18 months post-RT, while those with mild urinary symptoms had a modest worsening of symptoms. RT to the pelvic lymph nodes was independently associated with a worsened one-year urinary function score. These data can help inform patient expectations following RT.
Source of Funding: None

.jpg)
.jpg)