Back
Poster, Podium & Video Sessions
Podium
PD45: Benign Prostatic Hyperplasia: Surgical Therapy & New Technology IV
PD45-10: Outcomes after Holmium Laser Enucleation of the prostate, Open Simple Prostatectomy, and Robotic Simple Prostatectomy: Experience from a large academic medical center
Sunday, May 15, 2022
2:30 PM – 2:40 PM
Location: Room 252
Matthew Lee*, Meera Ganesh, Joshua Han, Quan Mai, Mark Assmus, Jessica Helon, Chicago, IL, Briana Kaplunov, Philadelphia, PA, Amy Krambeck, Chicago, IL
- ML
Matthew Lee, MD
Endourology Fellow at Northwestern University
Northwestern University
Podium Presenter(s)
Introduction: Per AUA guidelines, large prostates (defined as =80g in size) can be managed with Holmium Laser Enucleation of the Prostate (HoLEP), Open simple prostatectomy (OSP) or robotic simple prostatectomy (RSP). While these modalities have been previously compared to one another, one study only compared 32 RSPs to 600 HoLEPs. To our knowledge, the three modalities have never been compared against each other in the same cohort. Furthermore, in any published studies, the authors were not performing same-day catheter removal and discharge after HoLEP, indicating the studies must be updated. Herein, we present our experience performing HoLEP, OSP, and RSP for large prostates at a large academic medical center.
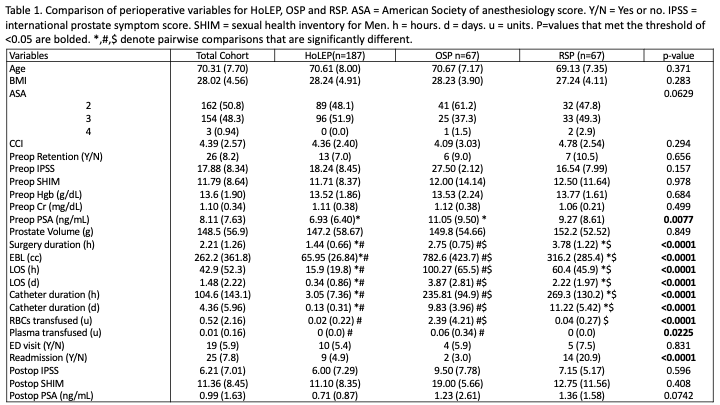
Methods: The Northwestern Enterprise Data Warehouse (EDW) is a system-wide electronic medical record based data platform. We queried the EDW for all patients undergoing HoLEP, OSP, and RSP from Jan 2011 to Oct 2021 for prostates =80g. Patients were identified by CPT code (52649, 55831/ 55821, 55899, respectively). Variables were abstracted from the EDW and medical record. Statistical analysis was performed using SAS studio (2021). Multiple comparisons for continuous variables were performed using ANOVA with Tukey’s corrections. Chi-square tests were used for categorical variables. P-value <0.05 was determined to be statistically significant.
Results: The three cohorts were similar in age, BMI, and Carlson comorbidity index. There was no difference in preoperative Hgb, Cr or prostate volume. PSA was higher in the OSP group (p=0.0077). Surgery duration, estimated blood loss (EBL), length of stay (LOS) and catheter duration were all shortest in the HoLEP group (p < 0.0001). OSP had the highest EBL and HoLEP had the lowest EBL (P <0.0001) which also translated into less RBC transfusions for HoLEP and RSP compared to OSP (p < 0.0001). There were no differences in ED visits, but RSP had the highest readmission rate (p < 0.0001).
Conclusions: In this cohort where HoLEP patients underwent same-day catheter removal and discharge, despite similar preoperative characteristics, HoLEP was associated with shorter surgery duration, LOS and catheter duration. HoLEP also had the lowest EBL and RBCs transfused with an increase in ED visits or readmissions.
Source of Funding: None
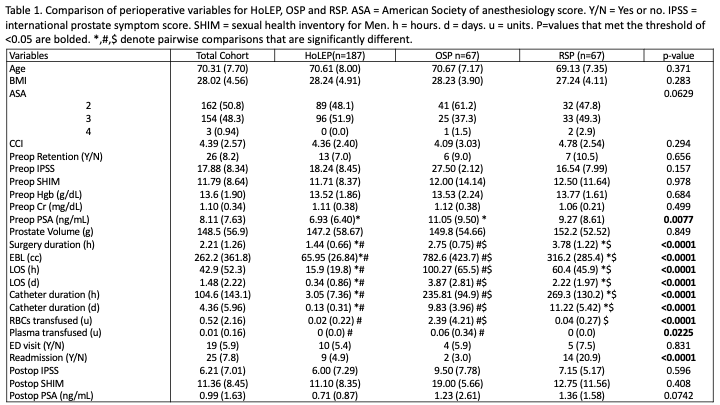
Methods: The Northwestern Enterprise Data Warehouse (EDW) is a system-wide electronic medical record based data platform. We queried the EDW for all patients undergoing HoLEP, OSP, and RSP from Jan 2011 to Oct 2021 for prostates =80g. Patients were identified by CPT code (52649, 55831/ 55821, 55899, respectively). Variables were abstracted from the EDW and medical record. Statistical analysis was performed using SAS studio (2021). Multiple comparisons for continuous variables were performed using ANOVA with Tukey’s corrections. Chi-square tests were used for categorical variables. P-value <0.05 was determined to be statistically significant.
Results: The three cohorts were similar in age, BMI, and Carlson comorbidity index. There was no difference in preoperative Hgb, Cr or prostate volume. PSA was higher in the OSP group (p=0.0077). Surgery duration, estimated blood loss (EBL), length of stay (LOS) and catheter duration were all shortest in the HoLEP group (p < 0.0001). OSP had the highest EBL and HoLEP had the lowest EBL (P <0.0001) which also translated into less RBC transfusions for HoLEP and RSP compared to OSP (p < 0.0001). There were no differences in ED visits, but RSP had the highest readmission rate (p < 0.0001).
Conclusions: In this cohort where HoLEP patients underwent same-day catheter removal and discharge, despite similar preoperative characteristics, HoLEP was associated with shorter surgery duration, LOS and catheter duration. HoLEP also had the lowest EBL and RBCs transfused with an increase in ED visits or readmissions.
Source of Funding: None

.jpg)
.jpg)