Back
Poster, Podium & Video Sessions
Podium
PD47: Sexual Function/Dysfunction: Evaluation II
PD47-01: Low Socioeconomic Status Is a Risk Factor for Erectile Dysfunction: An Analysis of NHANES Data
Sunday, May 15, 2022
1:00 PM – 1:10 PM
Location: Room 245
Eric Macdonald*, Lake Success, NY, Joseph Kim, Bronx, NY, Darius A. Paduch, Lake Success, NY

Eric J. Macdonald
The Smith Institute for Urology
Podium Presenter(s)
Introduction: Socioeconomic status (SES) plays a critical role in an individual’s overall health. However, little is known about the relationship between SES and erectile dysfunction (ED), a condition that affects millions of men in the United States. We analyzed nationally representative survey data to determine the effect of SES on ED.
Methods: Data was obtained from the National Health and Nutrition Examination Survey (NHANES). Demographic, medical, laboratory, and social factors were collected. Age matching was performed due to significantly different mean ages among men of different races. SES was estimated using the poverty income ratio (PIR), a ratio of family income to established poverty levels. Low SES was defined by PIR <2. Erectile function was assessed from a single survey question: “How would you describe your ability to get and keep an erection adequate for satisfactory sexual intercourse?” Responses were divided into two groups: normal (always and usually able to maintain an erection) and ED (sometimes or never able to maintain an erection). Weighted prevalence comparisons were performed using Chi-squared and t-tests at p=0.05. Multivariate logistic regression was subsequently used to characterize the interplay between well-established risk factors for ED and SES.
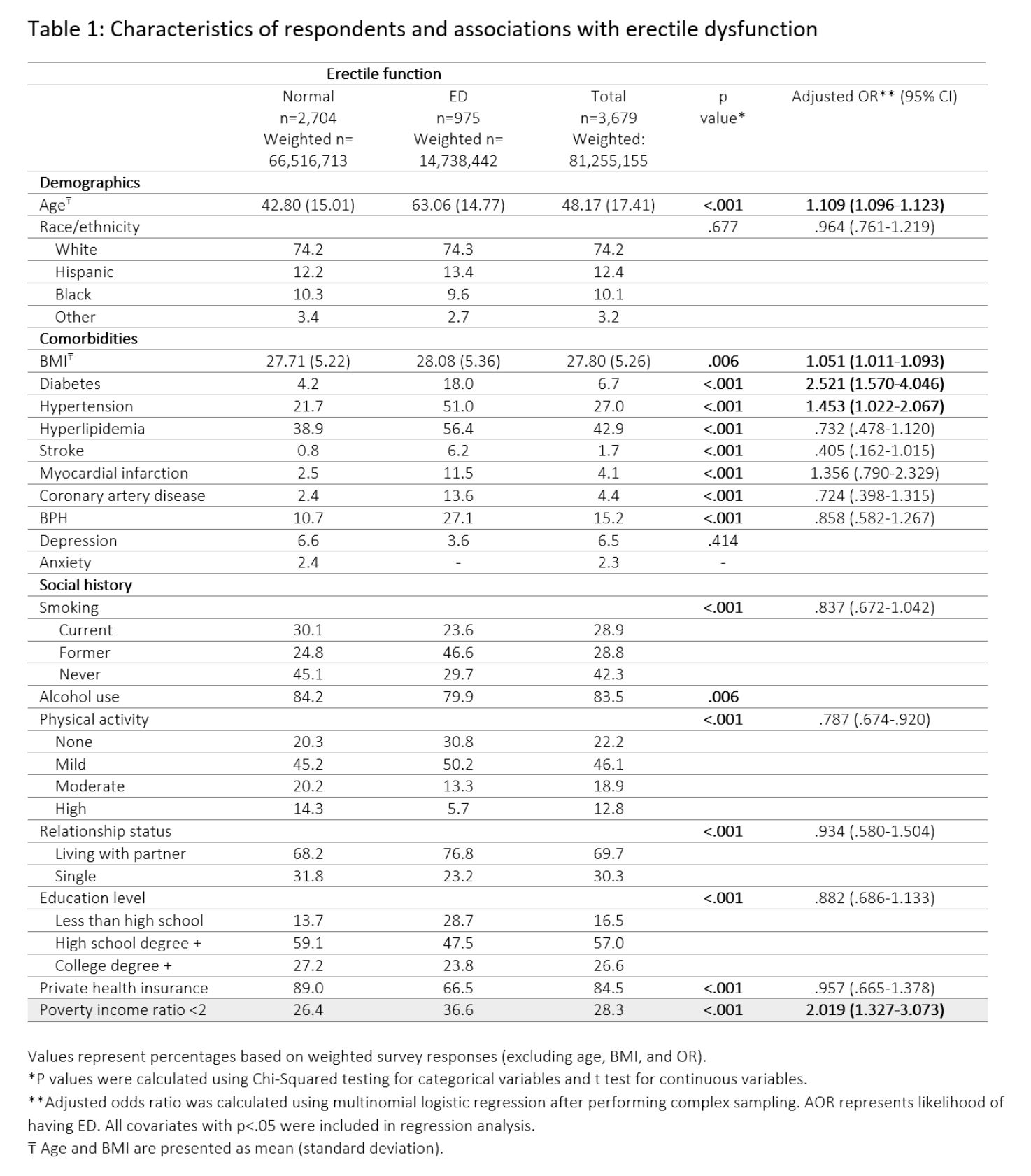
Results: 3,898 men responded to the ED survey question. After age matching, 3,679 men (mean age 48.14 ±17.41) were included. 975 men (26.5%) reported ED. Weighted prevalence comparisons are reported in Table 1 with many factors showing a significant association (p <.05) with ED. Multivariate logistic regression showed that patients with a low income (PIR <2) were significantly more likely to report ED; AOR=2.02 (1.33-3.07; p<0.001). Only diabetes had a similar AOR of 2.52 (1.57-4.05, p<0.001). Other social factors, such as private insurance coverage and education level, did not maintain significance during multivariate regression analysis.
Conclusions: This study provides strong evidence that low SES is an independent risk factor for ED. Physicians must consider SES when evaluating patients with ED and forming a treatment plan. Our data suggest that future urological outcome studies must include SES as an important modifying factor to ensure accurate analysis.
Source of Funding: None
Methods: Data was obtained from the National Health and Nutrition Examination Survey (NHANES). Demographic, medical, laboratory, and social factors were collected. Age matching was performed due to significantly different mean ages among men of different races. SES was estimated using the poverty income ratio (PIR), a ratio of family income to established poverty levels. Low SES was defined by PIR <2. Erectile function was assessed from a single survey question: “How would you describe your ability to get and keep an erection adequate for satisfactory sexual intercourse?” Responses were divided into two groups: normal (always and usually able to maintain an erection) and ED (sometimes or never able to maintain an erection). Weighted prevalence comparisons were performed using Chi-squared and t-tests at p=0.05. Multivariate logistic regression was subsequently used to characterize the interplay between well-established risk factors for ED and SES.
Results: 3,898 men responded to the ED survey question. After age matching, 3,679 men (mean age 48.14 ±17.41) were included. 975 men (26.5%) reported ED. Weighted prevalence comparisons are reported in Table 1 with many factors showing a significant association (p <.05) with ED. Multivariate logistic regression showed that patients with a low income (PIR <2) were significantly more likely to report ED; AOR=2.02 (1.33-3.07; p<0.001). Only diabetes had a similar AOR of 2.52 (1.57-4.05, p<0.001). Other social factors, such as private insurance coverage and education level, did not maintain significance during multivariate regression analysis.
Conclusions: This study provides strong evidence that low SES is an independent risk factor for ED. Physicians must consider SES when evaluating patients with ED and forming a treatment plan. Our data suggest that future urological outcome studies must include SES as an important modifying factor to ensure accurate analysis.
Source of Funding: None

.jpg)
.jpg)