Back
Poster, Podium & Video Sessions
MP01: Benign Prostatic Hyperplasia: Surgical Therapy & New Technology I
MP01-05: Prostatic artery embolization compared to trans-urethral resection of the prostate and prostatic urethral lift: A real-world population-based study
Friday, May 13, 2022
7:00 AM – 8:15 AM
Location: Room 228
Brendan L. Raizenne*, Montréal, Canada, Xinyan Zheng, New York, NY, Kussil Oumedjbeur, Montreal, Canada, Jialin Mao, New York, NY, Kevin C. Zorn, Montréal, Canada, Dean Elterman, Toronto, Canada, Naeem Bhojani, Montréal, Canada, Art Sedrakyan, Bilal Chughtai, New York, NY

Brendan Lapointe Raizenne, MD, BS
University of Montreal
Poster Presenter(s)
Introduction: Growing interests for minimally invasive surgical techniques (MISTs) for the treatment of benign prostatic hyperplasia (BPH) associated lower urinary tract symptoms (LUTS) have emerged. Prostatic artery embolization (PAE) is a novel MISTs utilizing selective angioembolization of prostatic arteries to treat LUTS/BPH. However, real-world data comparing surgical outcomes between MISTs and resection techniques is lacking. We assessed the differences in surgical outcomes between PAE, Transurethral resection of the prostate (TURP) and Prostatic Urethral Lift (PUL) in a real world-population for LUTS/BPH.
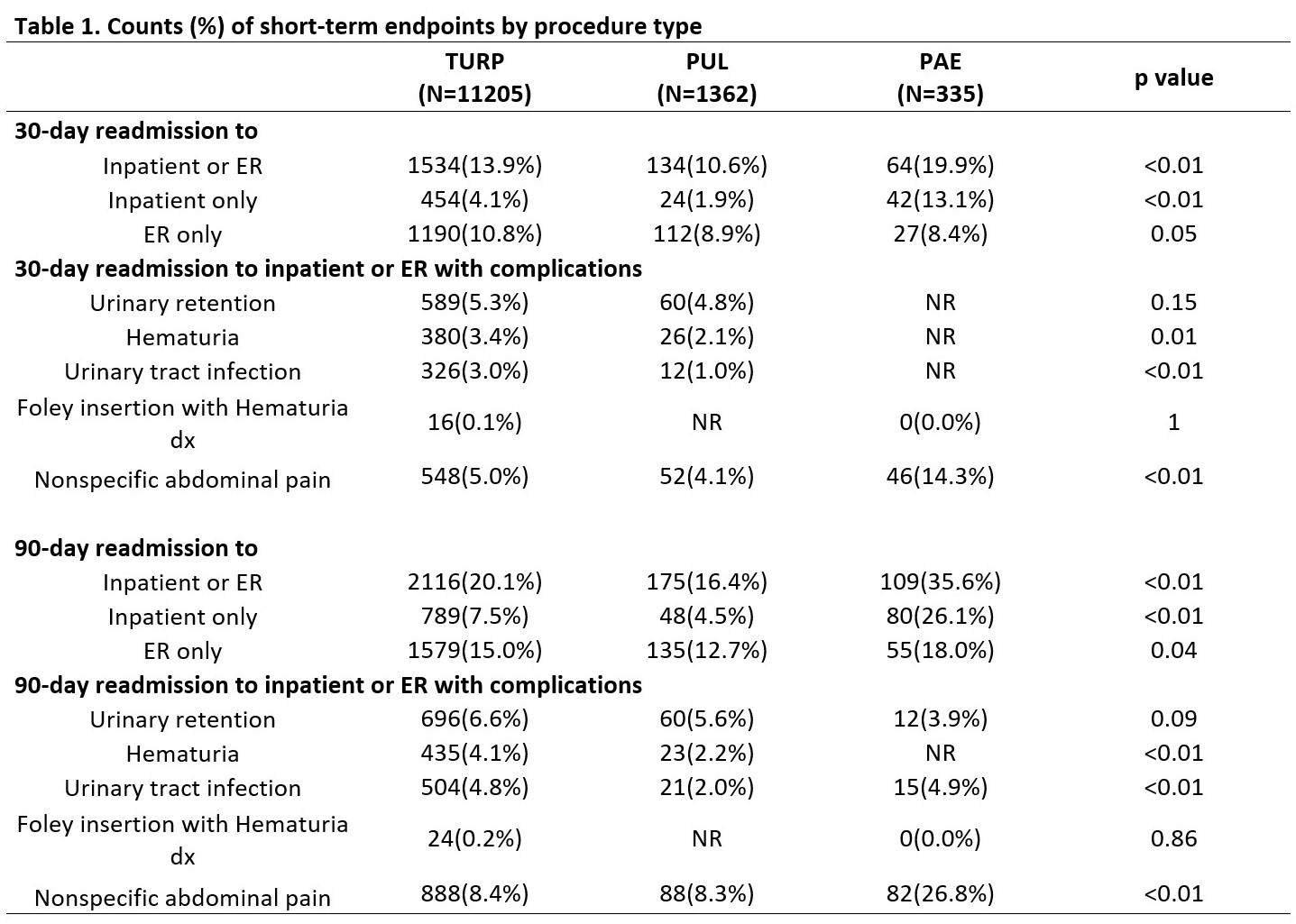
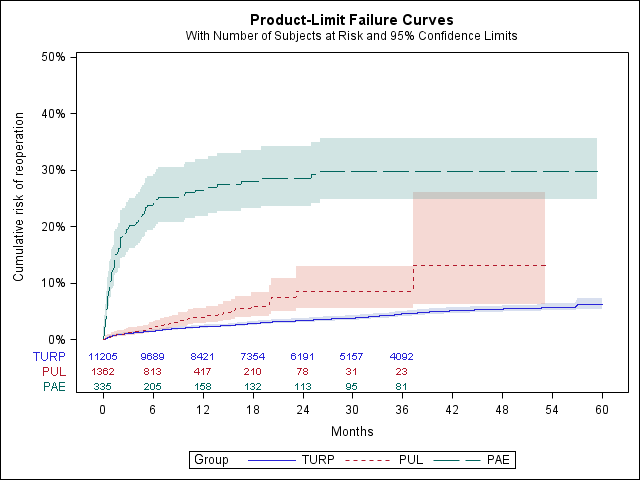
Methods: We present an observational population-based study of 12,902 men with BPH in New York State who received PAE, TURP and PUL in outpatient and ambulatory surgery settings from 2014 to 2018. For short term outcomes, we reported 30-day and 90-day readmission risks to inpatient and emergency room (ER) with/without complications and compared them using Chi-square tests and mixed effect logistic regressions. For long term outcomes, we reported retreatment and stricture rates using Kaplan Meier failure curves and compared them using Log rank tests and Cox regression models.
Results: Of 12,902 men, 335 had PAE, 11,205 had TURP and 1,362 had PUL. PAE exhibited the highest 30-day (19.9%) and 90-day (35.6%) readmission risk to inpatient or ER (p < 0.05). Non-specific abdominal pain was the main complication for 30-day and 90-day readmission to inpatient or ER for PAE (14.3% and 26.8%, respectively). After 2 years of follow-up, PAE exhibited the highest retreatment rate with 28.5% (95%CI: 23.7%-34.2%) compared to TURP (3.4% (95%CI: 3.1%-3.8%)) and PUL (8.5% (95%CI: 5.6%-12.9%)) (p < 0.001). No PAE patients had stricture.
Conclusions: In a real-world population, PAE exhibited the highest 30-day and 90-day readmission to inpatient or ER and the highest retreatment rate for all surgical techniques. Further studies should focus on identifying what type of patient would benefit the most from PAE.
Source of Funding: None
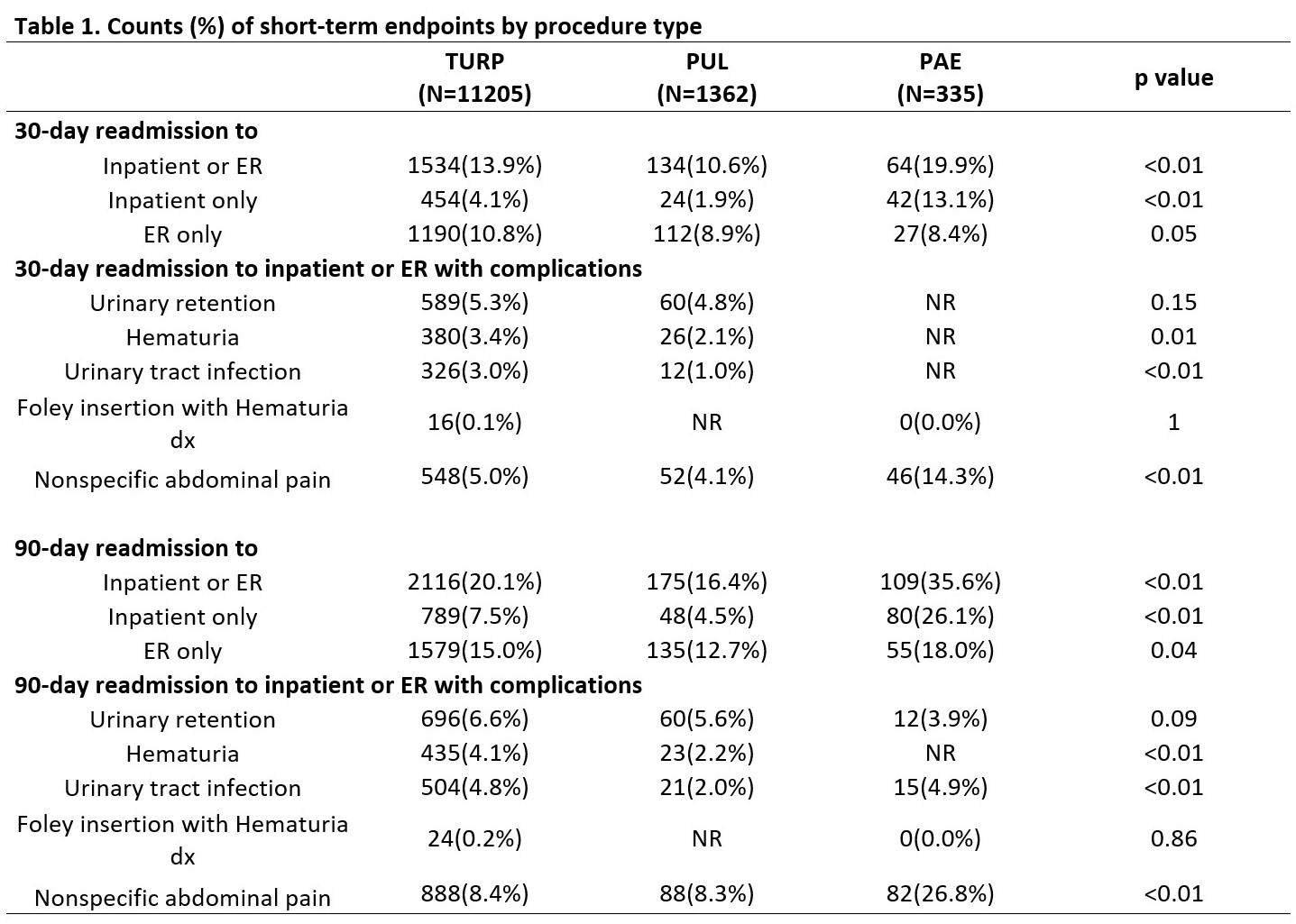
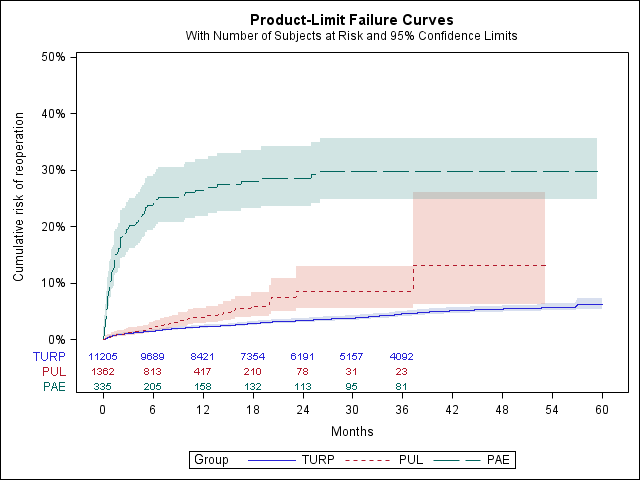
Methods: We present an observational population-based study of 12,902 men with BPH in New York State who received PAE, TURP and PUL in outpatient and ambulatory surgery settings from 2014 to 2018. For short term outcomes, we reported 30-day and 90-day readmission risks to inpatient and emergency room (ER) with/without complications and compared them using Chi-square tests and mixed effect logistic regressions. For long term outcomes, we reported retreatment and stricture rates using Kaplan Meier failure curves and compared them using Log rank tests and Cox regression models.
Results: Of 12,902 men, 335 had PAE, 11,205 had TURP and 1,362 had PUL. PAE exhibited the highest 30-day (19.9%) and 90-day (35.6%) readmission risk to inpatient or ER (p < 0.05). Non-specific abdominal pain was the main complication for 30-day and 90-day readmission to inpatient or ER for PAE (14.3% and 26.8%, respectively). After 2 years of follow-up, PAE exhibited the highest retreatment rate with 28.5% (95%CI: 23.7%-34.2%) compared to TURP (3.4% (95%CI: 3.1%-3.8%)) and PUL (8.5% (95%CI: 5.6%-12.9%)) (p < 0.001). No PAE patients had stricture.
Conclusions: In a real-world population, PAE exhibited the highest 30-day and 90-day readmission to inpatient or ER and the highest retreatment rate for all surgical techniques. Further studies should focus on identifying what type of patient would benefit the most from PAE.
Source of Funding: None

.jpg)
.jpg)