Back
Poster, Podium & Video Sessions
MP02: Infections/Inflammation/Cystic Disease of the Genitourinary Tract: Kidney & Bladder I
MP02-20: Decreased risk of urinary infection is associated with single use ureteroscopes
Friday, May 13, 2022
7:00 AM – 8:15 AM
Location: Room 225
Rei Unno*, Xavier Cortez, Leslie Charondo, Kevin Chang, Nizar Hakam, Carter Chan, Heiko Yang, Gregory Hosier, Fadl Hamouche, David Bayne, Marshall Stoller, Thomas Chi, San Francisco, CA
- RU
Poster Presenter(s)
Introduction: Although single-use ureteroscopes have been shown to be comparable with reusable ureteroscopes in terms of intraoperative maneuverability, visual image quality, as well as stone-related clinical outcomes, there are few large scale reports regarding clinical outcomes related to single-use ureteroscopes. In the current study, we aimed to understand the impact of single-use ureteroscopes on clinical outcomes for ureteroscopic stone removal and whether their use reduced postoperative urinary tract infection (UTI) risk.
Methods: This was a single-center, retrospective cohort study designed to compare single-use with reusable flexible ureteroscopes regarding peri- and postoperative outcomes between June 2012 and March 2021. The primary endpoint was postoperative UTI. The secondary endpoints were intraoperative outcomes (operative time and stone clearance), perioperative complications, hospitalization time, and re-presentation to the hospital (telephone call, ED visit, and re-admission) after URS.
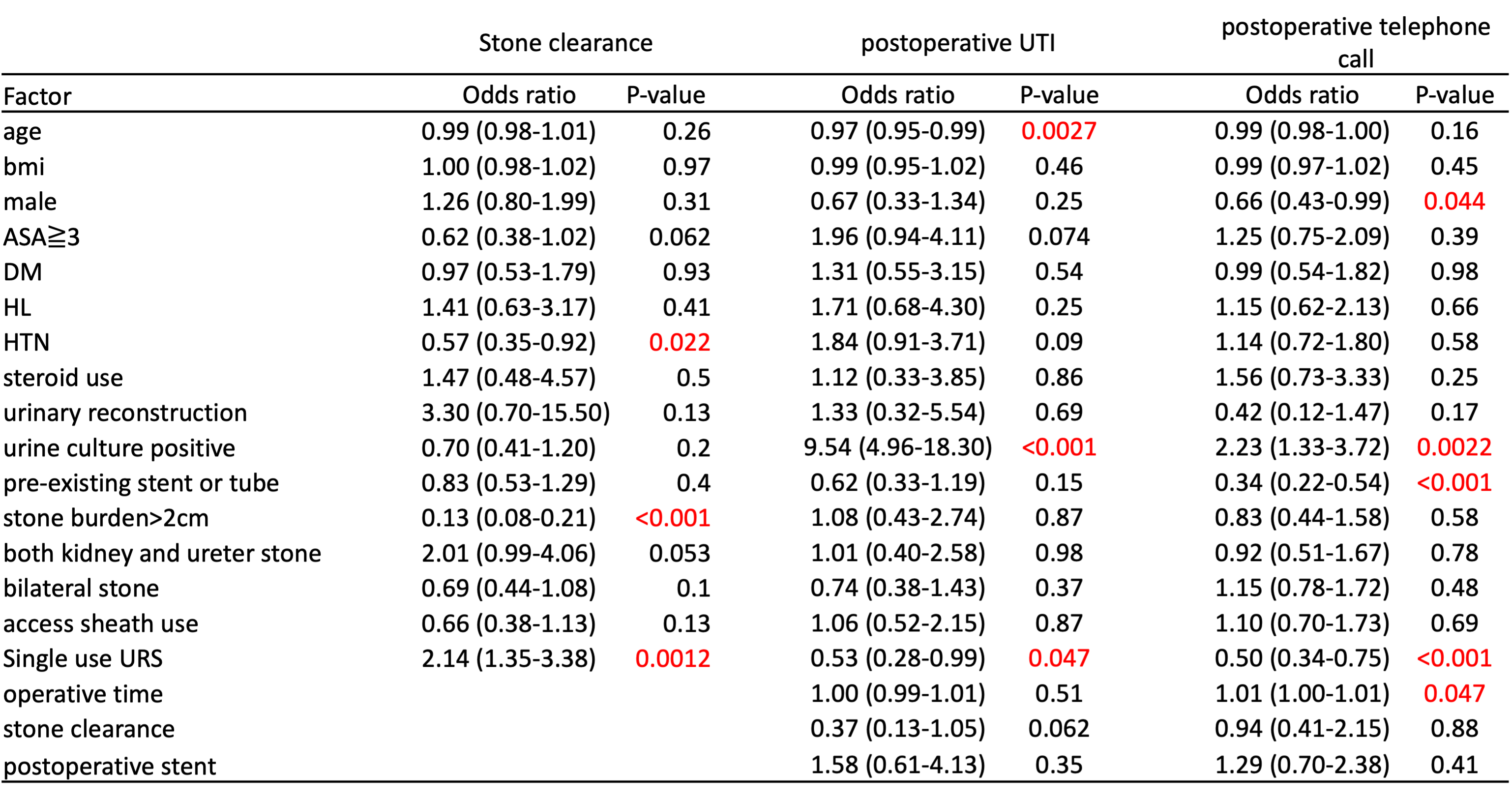
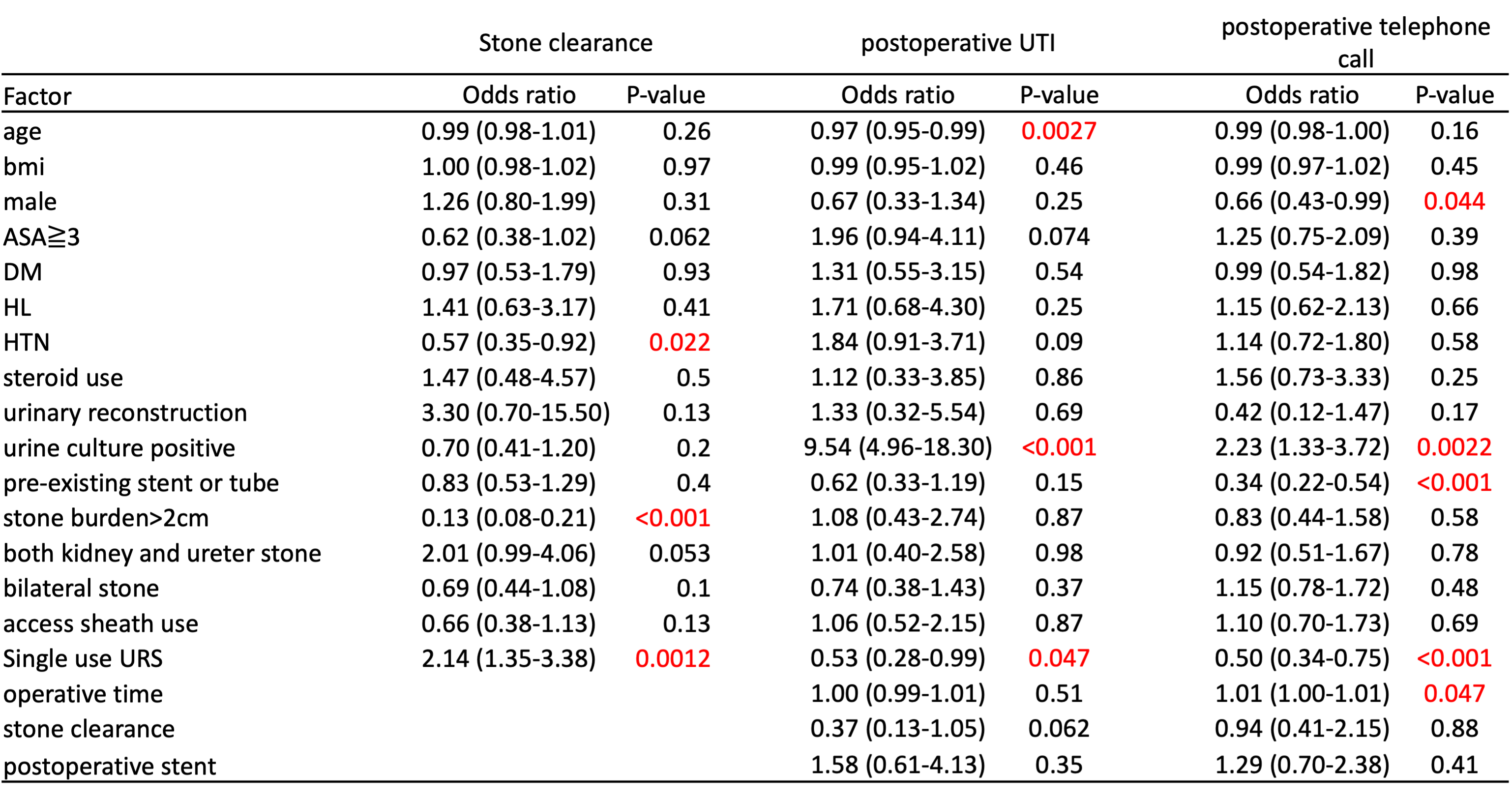
Results: A total of 991 patients were analyzed, 500 patients in the single-use URS group (50.4%) and 491 patients in the reusable group (49.6%). On univariate analysis, patients in the single-use URS group were more often male and had lower BMI and presented with more bilateral stones than those in the reusable group. Single-use URS was associated with a lower chance of postoperative UTI (6.5% vs 11.9%, p=0.018) as well as a higher stone clearance rate (90.0% vs 83.9%, p=0.005) and fewer postoperative telephone calls (19.2% vs 29.2%, p=0.002). There were no significant differences in operative time, perioperative complications, ED visits, and re-admission between the two groups. On multivariate analysis, single-use URS remained a strong factor associated with stone clearance rate and decreased risk of postoperative UTI and postoperative telephone calls (Table 1). Postoperative sepsis, perioperative complications, and re-admission were associated with a positive preoperative urine culture.
Conclusions: These data show that the single-use URS is beneficial in reducing postoperative UTI and telephone calls as well as increasing the stone clearance rate. These results provide a clinical justification for their routine use during ureteroscopic stone removal.
Source of Funding: none
Methods: This was a single-center, retrospective cohort study designed to compare single-use with reusable flexible ureteroscopes regarding peri- and postoperative outcomes between June 2012 and March 2021. The primary endpoint was postoperative UTI. The secondary endpoints were intraoperative outcomes (operative time and stone clearance), perioperative complications, hospitalization time, and re-presentation to the hospital (telephone call, ED visit, and re-admission) after URS.
Results: A total of 991 patients were analyzed, 500 patients in the single-use URS group (50.4%) and 491 patients in the reusable group (49.6%). On univariate analysis, patients in the single-use URS group were more often male and had lower BMI and presented with more bilateral stones than those in the reusable group. Single-use URS was associated with a lower chance of postoperative UTI (6.5% vs 11.9%, p=0.018) as well as a higher stone clearance rate (90.0% vs 83.9%, p=0.005) and fewer postoperative telephone calls (19.2% vs 29.2%, p=0.002). There were no significant differences in operative time, perioperative complications, ED visits, and re-admission between the two groups. On multivariate analysis, single-use URS remained a strong factor associated with stone clearance rate and decreased risk of postoperative UTI and postoperative telephone calls (Table 1). Postoperative sepsis, perioperative complications, and re-admission were associated with a positive preoperative urine culture.
Conclusions: These data show that the single-use URS is beneficial in reducing postoperative UTI and telephone calls as well as increasing the stone clearance rate. These results provide a clinical justification for their routine use during ureteroscopic stone removal.
Source of Funding: none

.jpg)
.jpg)