Back
Poster, Podium & Video Sessions
Moderated Poster
MP09: Prostate Cancer: Detection & Screening I
MP09-10: Quantification of Perineural Invasion by Prostate Cancer on Needle Core Biopsy: Implication for Risk Stratification
Friday, May 13, 2022
10:30 AM – 11:45 AM
Location: Room 222
Yuki Teramoto, Ying Wang, Hiroshi Miyamoto*, Rochester, NY
Hiroshi Miyamoto, MD, PhD
University of Rochester Medical Center
Poster Presenter(s)
Introduction: Perineural invasion (PNI) on prostate biopsy (Bx) has been considered as a key prognosticator. However, it remains unclear how the number of actual PNI foci impacts on patient outcome. We herein quantified PNI in Bx specimens with the aim of creating a simple index for prognostic prediction.
Methods: We assessed consecutive 152 patients exhibiting PNI on systematic sextant Bx, but not on targeted Bx, followed by radical prostatectomy (RP) both at our institution from 2009 to 2016.
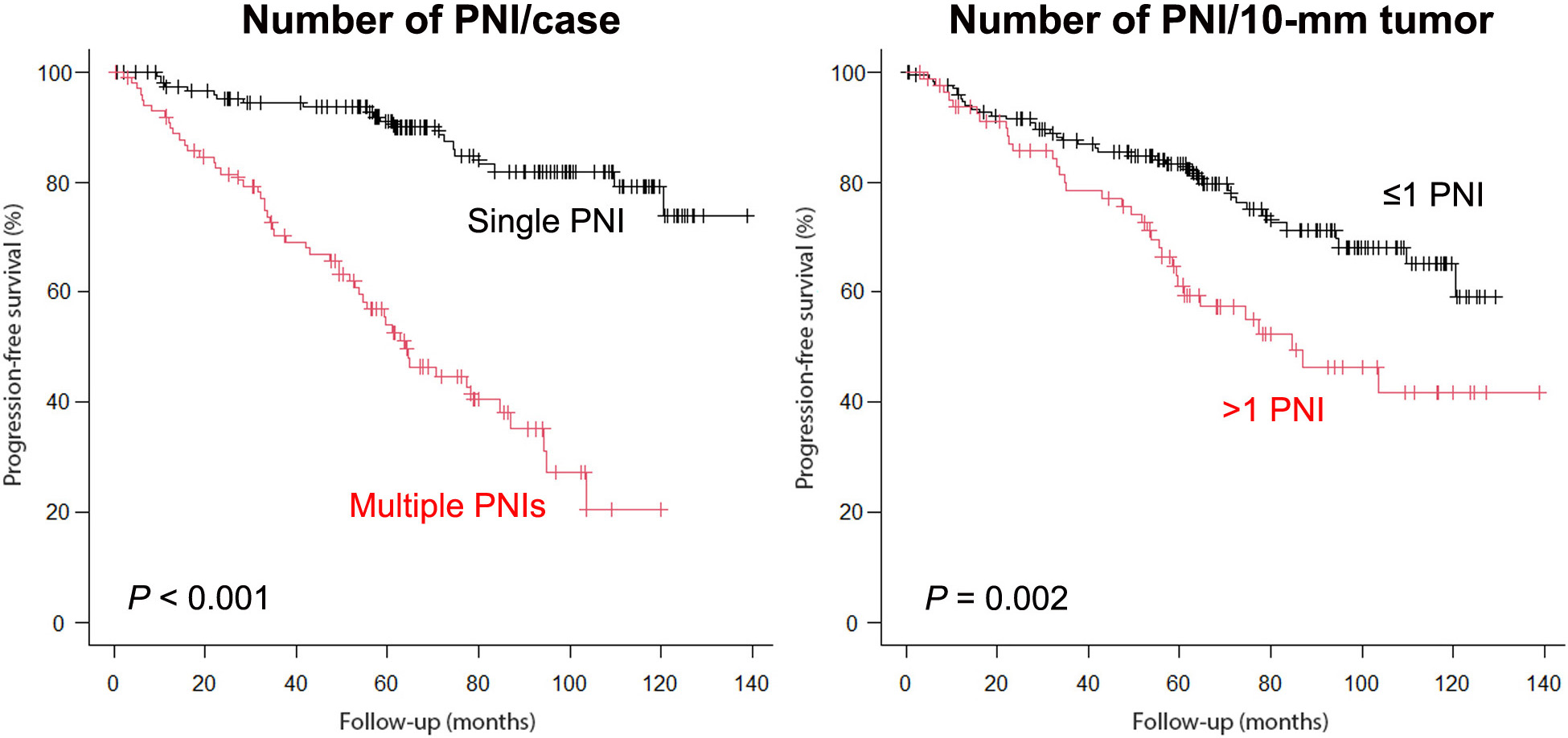
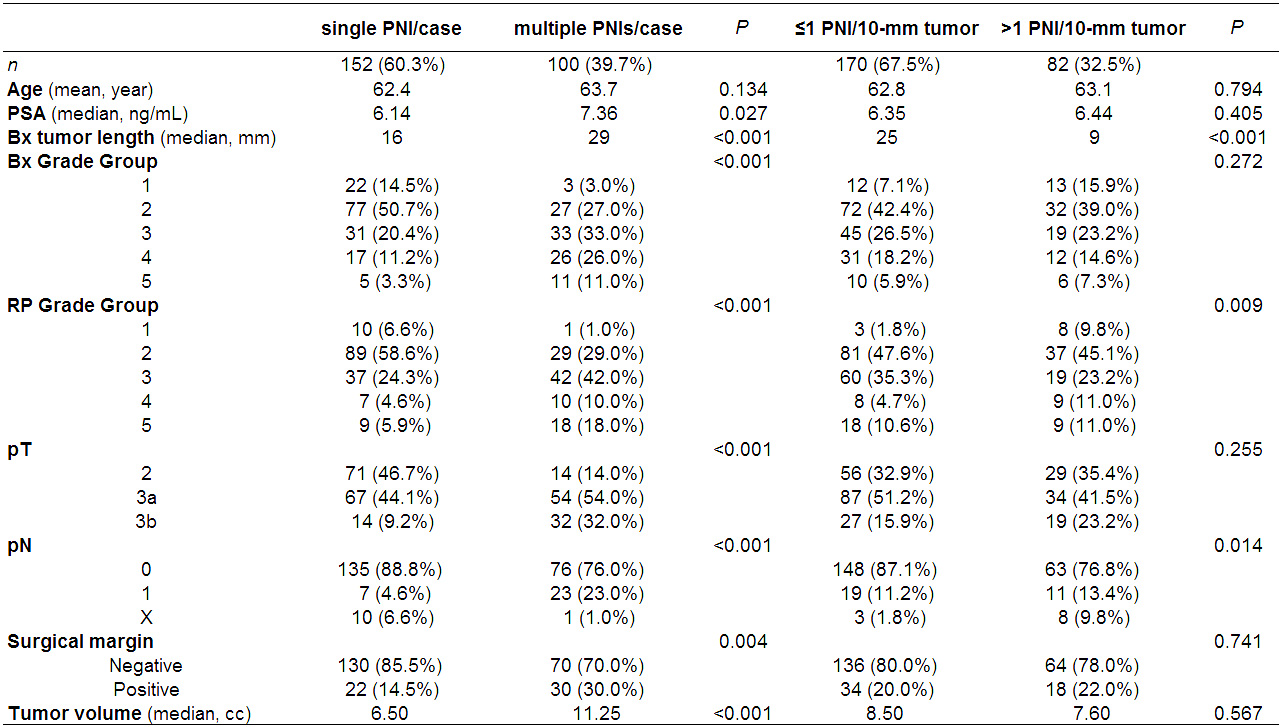
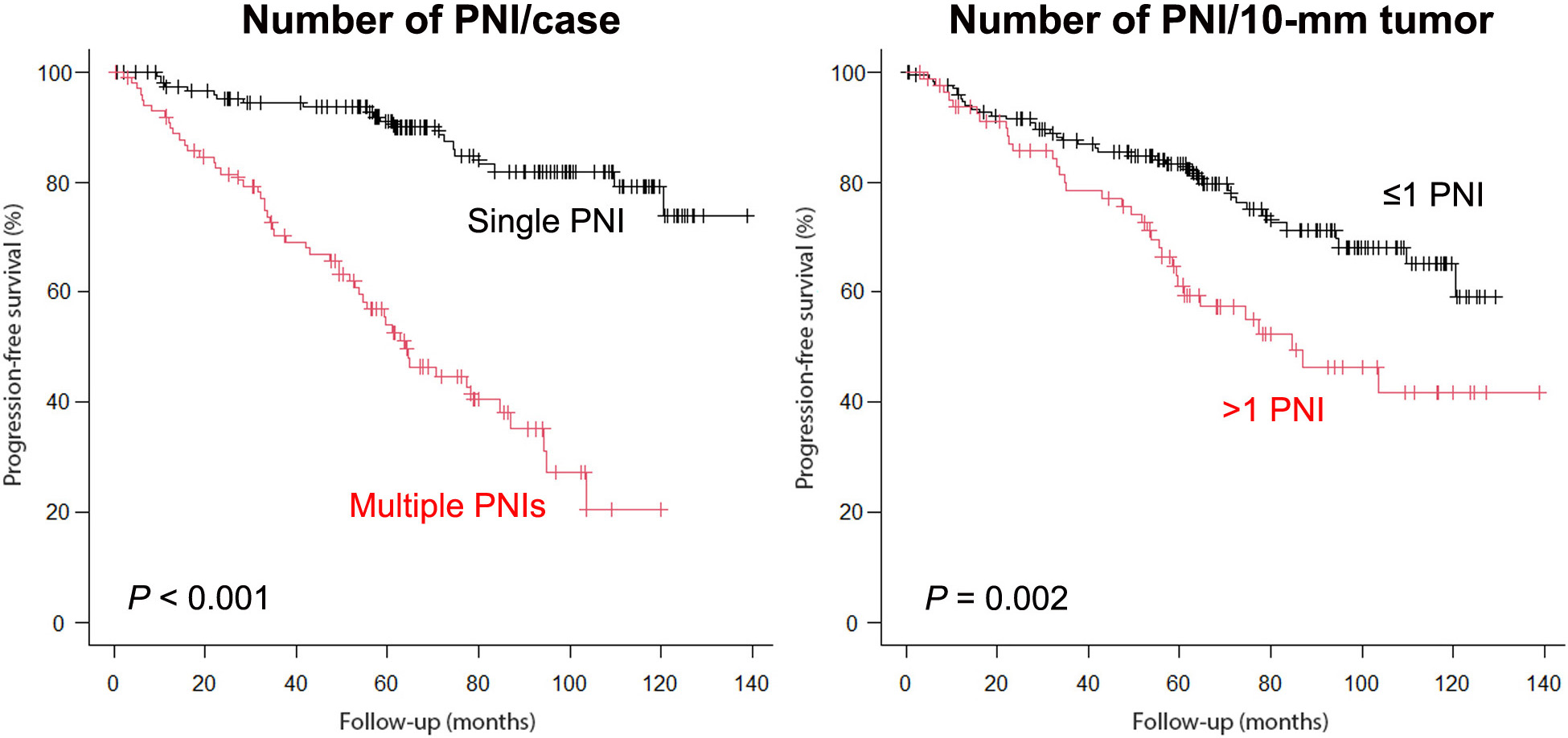
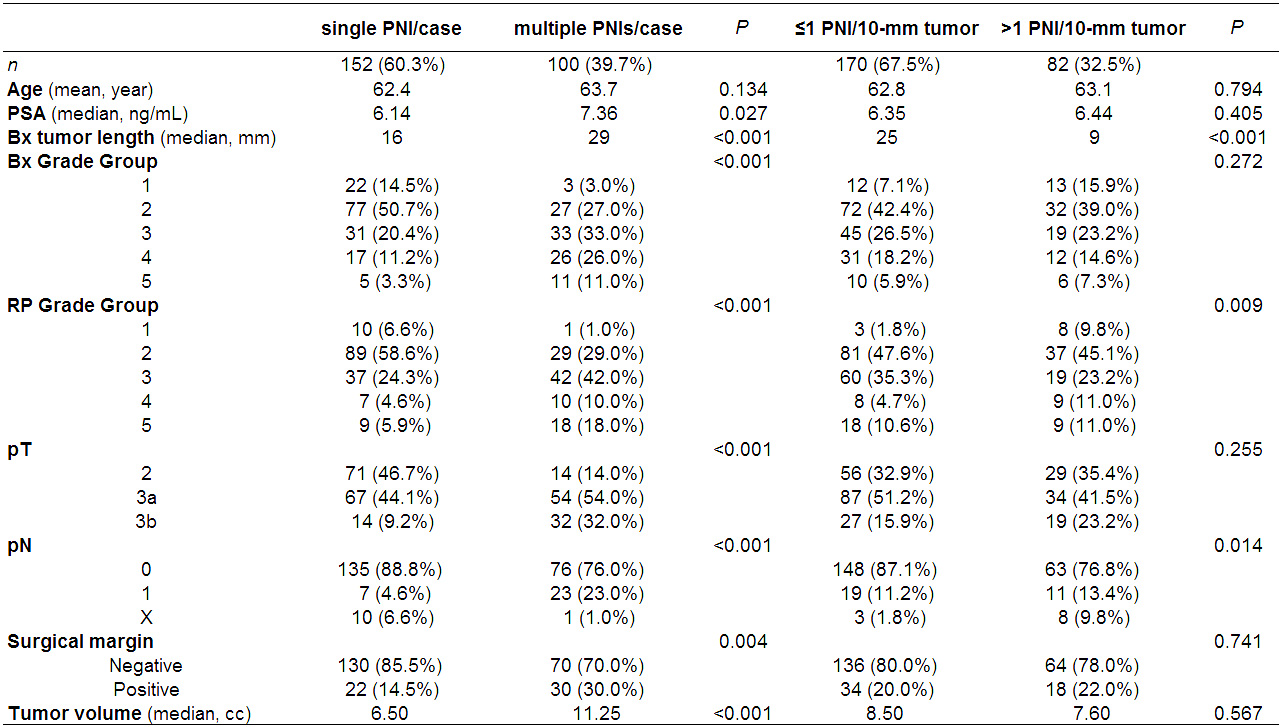
Results: Only 1 PNI in the entire specimen was present in 152 (60.3%) cases, while other cases showed 2 [53 (21.0%)], 3 [19 (7.5%)], 4 [12 (4.8%)], or 5-10 [16 (6.3%)] PNIs. Compared to cases with a single PNI, multiple PNIs were significantly associated with higher PSA, higher Grade Group (GG) on Bx or RP, higher pT/pN category, positive surgical margin, and larger tumor volume. When total tumor length on each Bx was considered, significant differences in GG on RP and pN status between cases with =1 vs. >1 PNI per 10-mm tumor were observed. Kaplan-Meier analysis revealed a significantly higher risk of progression in patients with multiple PNIs (vs. a single PNI per Bx) as well as those with >1 PNI per 10-mm tumor (vs. =1 PNI). Significant differences in progression-free survival (PFS) between =1 vs. >1 PNI/10-mm tumor were also seen in subgroups, including those with =10-mm tumor (P=0.021), >10/=20-mm tumor (P <0.001), and >20-mm tumor (P=0.005), and those showing PNI only at 1 sextant site (P=0.029). When the cohort was divided into 3 groups (i.e. 1 vs. 2 vs. 3-10 PNI/case, =1 vs. >1/=2 vs. >2 PNI/10-mm tumor), significant differences in PFS were still seen. In multivariate analysis, both multiple PNIs/case (HR=4.533, P<0.001) and >1 PNI/10-mm tumor (HR=2.863, P<0.001) showed significance for progression.
Conclusions: =2 PNI foci and >1 PNI per 10-mm tumor on each Bx were found to be associated with poor prognosis, as independent predictors, in those undergoing RP. Remarkably, the prognostic impact of the latter remained significant in all subgroups of patients examined.
Source of Funding: None
Methods: We assessed consecutive 152 patients exhibiting PNI on systematic sextant Bx, but not on targeted Bx, followed by radical prostatectomy (RP) both at our institution from 2009 to 2016.
Results: Only 1 PNI in the entire specimen was present in 152 (60.3%) cases, while other cases showed 2 [53 (21.0%)], 3 [19 (7.5%)], 4 [12 (4.8%)], or 5-10 [16 (6.3%)] PNIs. Compared to cases with a single PNI, multiple PNIs were significantly associated with higher PSA, higher Grade Group (GG) on Bx or RP, higher pT/pN category, positive surgical margin, and larger tumor volume. When total tumor length on each Bx was considered, significant differences in GG on RP and pN status between cases with =1 vs. >1 PNI per 10-mm tumor were observed. Kaplan-Meier analysis revealed a significantly higher risk of progression in patients with multiple PNIs (vs. a single PNI per Bx) as well as those with >1 PNI per 10-mm tumor (vs. =1 PNI). Significant differences in progression-free survival (PFS) between =1 vs. >1 PNI/10-mm tumor were also seen in subgroups, including those with =10-mm tumor (P=0.021), >10/=20-mm tumor (P <0.001), and >20-mm tumor (P=0.005), and those showing PNI only at 1 sextant site (P=0.029). When the cohort was divided into 3 groups (i.e. 1 vs. 2 vs. 3-10 PNI/case, =1 vs. >1/=2 vs. >2 PNI/10-mm tumor), significant differences in PFS were still seen. In multivariate analysis, both multiple PNIs/case (HR=4.533, P<0.001) and >1 PNI/10-mm tumor (HR=2.863, P<0.001) showed significance for progression.
Conclusions: =2 PNI foci and >1 PNI per 10-mm tumor on each Bx were found to be associated with poor prognosis, as independent predictors, in those undergoing RP. Remarkably, the prognostic impact of the latter remained significant in all subgroups of patients examined.
Source of Funding: None

.jpg)
.jpg)